 J Clin Aesthet Dermatol. 2018;11(8):41–44
J Clin Aesthet Dermatol. 2018;11(8):41–44
by Anwar Elawar, MD, and Serge Dahan, MD
Dr. Elawar is with the Aesthetic Dermatological Laser Center in Marseille, France. Dr. Dahan is with the St. Jean Languedoc Clinic in Toulouse, France.
Funding: No funding was provided.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Background. Severe scarring caused by acne is associated with substantial physical and psychological distress, both in adolescents and adults. There are two basic types of scars: atrophic (depressed) and raised (hypertrophic). Microneedle fractional radiofrequency (MFRF) is a new technology that uses extra sharp microneedles to heat the depths of the dermis, which promotes dermal collagen remodeling. In this study, we used electronically controlled non-insulated microneedle radiofrequency treatment to treat atrophic acne scars, improve skin texture, and reduce pore size.
Methods. Nineteen patients were enrolled in the study. The goal of the treatment was to improve acne scars and skin texture and to reduce pore size. Each patient received 2 to 6 treatments with one month intervals between treatments. Treated areas were visually assessed for skin response, including edema, erythema, and burns. We used the standard pain scale of 0 to 10 to assess pain during and after treatment.
Results. All the patients completed a series of 2 to 6 treatments. No adverse events as burns, scarring, or hyper/hypopigmentation were reported. Subjective pain assessment was the average point of 1.5, as reported by the patients. The subjective and objective questionnaire revealed high satisfaction from the treatment.
Conclusions. The presented study results show that the MFRF treatment provides a highly effective minimally invasive treatment for acne scars, skin texture improvement, and pore size reduction, with a short downtime and high subjective satisfaction rates.
Keywords: Radiofrequency, ENDYMED, 3DEEP®, Intensif, microneedles, fractional RF, wrinkle reduction, multisource, acne scars, skin texture
Introduction
Severe scarring caused by acne is associated with substantial physical and psychological distress, both in adolescents and adults.1 Atrophic acne scars can be subclassified into icepick, boxcar, and rolling scars. All three types might be observed on the same patient.2–4 Current treatments for depressed acne scars include chemical peels, dermabrasion, surgical excision, subcision, and laser treatments. These treatments all have their advantages and disadvantages.6 Additional common complaints in people with acne scars are changes in skin texture and color and enlarged pores size.5
Radiofrequency (RF) is a nonionizing electromagnetic radiation that has been used in medicine for nearly 100 years. In contrast to most lasers that target specific chromophores, RF is chromophore-independent. This allows significantly higher penetration into the skin and safe treatment of darker skin types.7–9
Microneedling fractional RF (MFRF) uses extra sharp microneedles to heat the depths of the dermis, promoting dermal collagen remodeling. Previous studies have demonstrated the efficacy of microneedle RF devices for skin tightening, wrinkle reduction, and acne scarring reduction. These studies reported that the MFRF treatment resulted in significantly less postinflammatory hyper- or hypopigmentation side effects compared to fractional CO2 lasers.10–20
The first generation of microneedle RF technology used insulated needles for skin rejuvenation and acne scars. The insulated needles allow energy flow throughout the noninsulated tip of the needle only, resulting in a small coagulated area in the dermis. Two disadvantages to the first-generation devices are significant microbleeding during the treatment and the need for several passes at different needle depths to treat the entire dermis depth.17,18
In this study, we used electronically controlled, noninsulated microneedle RF (Intensif applicator, EndyMed, Caesarea, Israel) to treat atrophic acne scars, improve skin texture, and reduce pore size. The needles are inserted into the skin using an electronically controlled, smooth motion motor, which is designed to minimize surface damage and patient discomfort. Using proprietary electronics, and the difference in impedance between the epidermis and the dermis, the MFRF device creates microzones of coagulation in the papillary and reticular dermis with minimal damage to the epidermis. RF emission delivered over the whole needle length allows better coagulation and heating of higher volumes of dermal tissue compared to insulated needles.21–22
Methods
Nineteen patients (13 women and 6 men), age 23 to 70 years (average 38±12.65), Skin Type II to IV were enrolled in the study. Inclusion criteria were healthy patients older than 18 years of age with depressed acne scars and the ability to comprehend and provide informed consent. Exclusion criteria were history of keloids, pregnancy or breastfeeding, clotting disorders, heart disorders, suspicious lesions on the treated area, permanent makeup or tattoo on the treatment area, autoimmune skin disorders, and refusal of posttreatment assessment. The goal of the treatment was to improve the appearance of acne scars and skin texture and reduce pore size. Informed consent to participate in the study and photoconsent for use of photos were received from all study participants. The study followed ethical principles described in the current revision of the Declaration of Helsinki.
Each patient received 2 to 6 treatments with a one-month interval between treatments. Follow-up sessions were performed one month and three months following the last treatment. Screening sessions were performed 10 to 20 days before the first treatment to assess skin reaction and to determine the treatment parameters. Each patient was treated with specific parameters according to the screening visit. Topical anesthesia was applied 30 to 60 minutes before the treatment. Facial areas were treated with a pulse duration of 110 to 140ms, 12 to 18W, and 2 to 3.5mm penetration depth. Each patient received 250 to 500 pulses per treatment. Treated areas were visually assessed for skin response, including edema, erythema, and burns. Patients were requested to assess the pain during the treatment using a scale of 0 to 10 (0=No pain, 10=Worst pain possible).
Posttreatment skin care regimen was consisted of soothing cream application on the treated area. Subjects were encouraged to a minimum of 30 sun protection factor (SPF) sunscreen throughout the course of the study along with their normal skin care regimen.
Photos were taken with VISIA CR camera (Canfield Scientific Inc., Fairfield, New Jersey, USA) and FotoFinder 2007, Mediscope (FotoFinder Systems, Columbia, Maryland) camera.
The attending physician and external observer (a board-certified dermatologist) evaluated the degree of improvement in acne scars and skin texture and pore size reduction, according to the Global Aesthetic Improvement Scale (GAIS): (0=No Improvement, 1=?25% Improvement [mild], 2=26–50% Improvement [moderate], 3=51–75% Improvement [good], 4=76–100% Improvement [excellent]).
Patients used the same scale to rate their subjective improvement. Patients were asked to specify if the treatment met their expectations and if they would recommend the treatment to their colleagues and/or friends.
Results


All the patients completed a series of 2 to 6 treatments. Mild-to-moderate erythema and edema was reported to occur following the treatment and lasted 2 to 5 hours. No adverse events (e.g., burns, scarring, or hyper/hypopigmentation) were reported. The average pain assessment score was 1.5 (0–10).
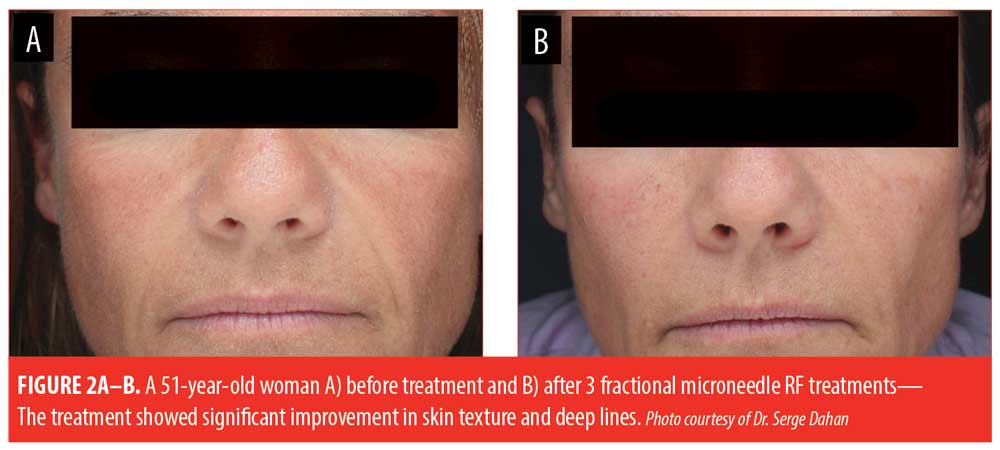
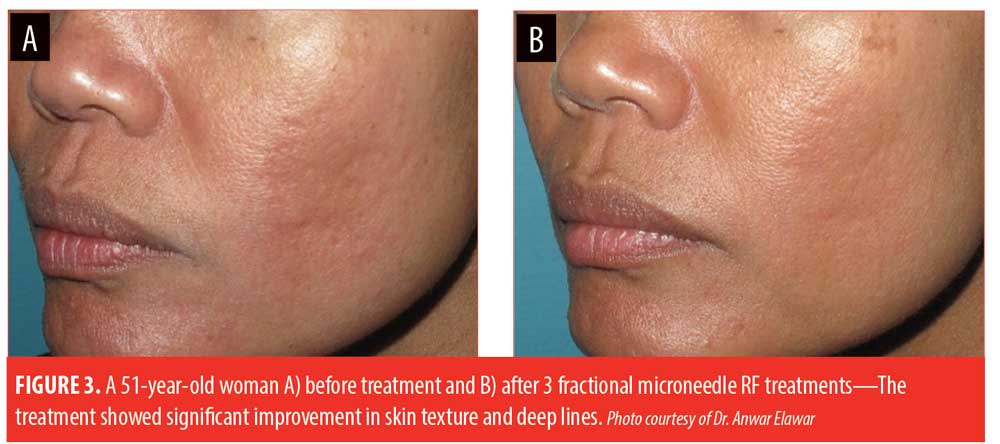
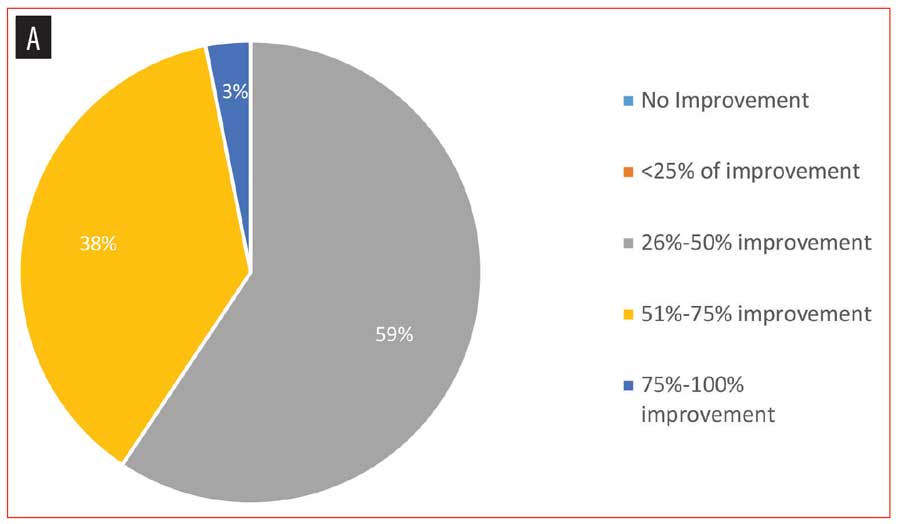
Patients reported overall satisfaction from the treatment. All of the patients reported a noticeable improvement—57.89 percent of the patients saw 51 to 75 percent improvement, 36.84 percent saw 26 to 50 percent improvement, and 5.26 percent saw 76 to 100 percent improvement (Figures 1–4). Additionally, 94 percent of patients said they would recommend the treatment to colleagues and/or friends.
Objective improvement in acne scars was graded by physician and the external observer. Both reported that 59.37 percent of patients saw 26 to 50 percent improvement in their acne scars, 37.5 percent saw 51 to 75 percent improvement, and 3.12 percent saw 76 to 100 percent improvement.
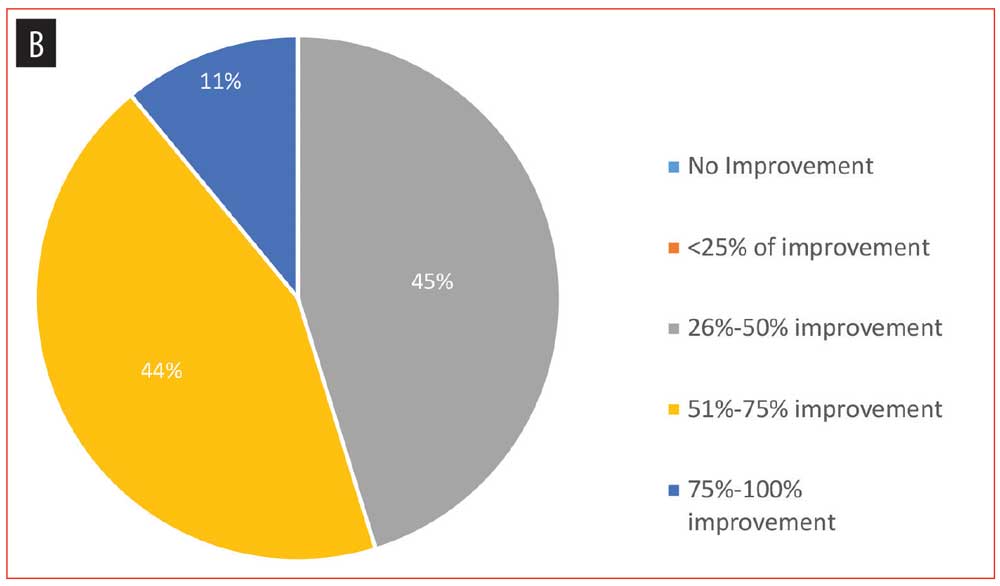
The degree of improvement in skin texture and pigmentation graded by physicians and external observer was 26 to 50 percent in 45.31 percent of patients, 51 to 75 percent in 43.75 percent of the patients, and 76 to 100 percent in 10.93 percent of the patients.
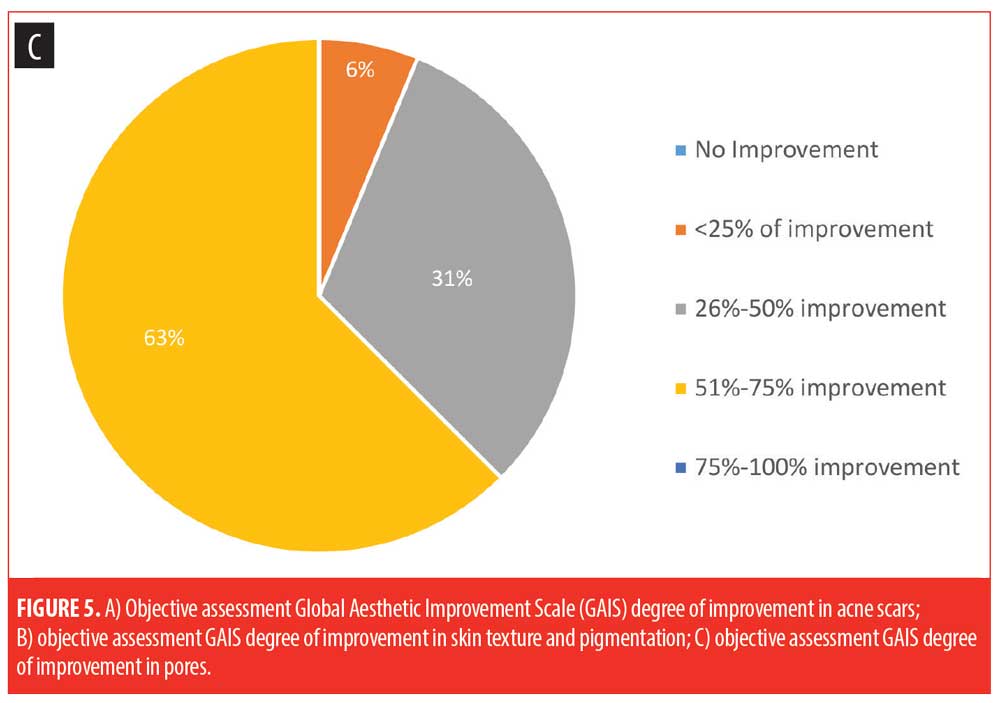
The degree of improvement in pores was 51 to 75 percent improvement in 62.5 percent of patients, 25 to 50 percent improvement in 31.25 percent of patients and less than 25 percent improvement in 6.25 percent of patients
(Figure 5).
Discussion
Harth et al21 studied the histological effect of the electronically controlled, noninsulated microneedle RF in vivo. Histology samples taken 4 and 14 days after the treatment show rapid epidermal renewal with proportional volume of coagulation in dermis related to the length of the needle and the power used.
The long-term skin tightening effect of the electronically controlled noninsulated microneedle RF treatment on Asian patients was studied by Tanaka et al.20 In this study, the authors reported long-term efficacy of skin tightening, using 3-D volumetric assessments with minimal complications and downtime.
Pudukadan et al14 reported the efficacy and safety of electronically controlled noninsulated RF microneedling system on atrophic acne scars in patients with dark skin (skin types III to V) with minimal pain or downtime.
In our study, we observed significant improvement in acne scars, skin texture, and pore size. The objective GAIS we observed moderate to excellent improvement in the appearance of acne scars and skin texture in 100 percent (N=19) of patients and moderate to excellent improvement in pore size in 93.75 percent of the patients.
The patients undergoing the treatment reported satisfaction with the results of the treatment, as measured subjectively using the same scale (GAIS).
The low level of reported pain might be attributed to the smooth motion and motorized needle insertion. The predefined depth of the needles in the dermis without epidermal coagulation reduces the risk of a postinflammatory hyper- or hypopigmentation (PIH). In the current study, no PIH, epidermal burns, or scar formation were observed.
Limitations. In this study, we had several limitations based on the sample size. Patient recruitment was challenging due to the fact that subjects are not always willing to attend follow-up visits. Long-term follow-up visits could serve to enlighten more changes on subjects’ skin. In some cases, there was a lack of available data from subject questionnaires. Future studies should include long-term follow-up visits of at least six months following the last treatment.
Conclusion
The noninsulated microneedle RF treatment was designed to allow controlled heating to a pre-defined dermal depth without epidermal coagulation. The smooth-motion, electronically controlled motor was designed to minimize trauma to the epidermis and decrease any discomfort to the patient. The RF microneedle treatment offers a minimally invasive treatment option with little downtime for the treatment of acne scars, improvement in skin texture, and reduced size of skin pores. Our results suggest this treatment offers high satisfaction in results among clinicians and patients. Random, controlled studies with a larger number of patients are needed to confirm our preliminary results.
References
- Shamban AT , Narurkar VA. Multimodal treatment of acne, acne scars and pigmentation. Dermatol Clin. 2009:27:459–471
- Layton AM, Henderson CA, Cunliffe J. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19(4):303–308.
- Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109–17.
- Cho SB, et al. Efficacy of the fractional photothermolysis system with dynamic operating mode on acne scars and enlarged facial pores. Dermatol Surg. 2009;35:
108–114. - Hellman J. Retrospective study of the use of a fractional radio frequency ablative device in the treatment of acne vulgaris and related acne scars. JCDSA. 2015;5:311–316.
- Elman M, Harth Y. Novel multi-source phase-controlled radiofrequency technology for nonablative and micro-ablative treatment of wrinkles, lax skin, and acne scars. Laser Ther. 2011;20:139–144.
- Ong MW, Bashir SJ. Fractional laser resurfacing for acne scars: a review. Br J Dermatol. 2012;166:1160–1169.
- Royo de la Torre J, Moreno-Moraga J, Estefania M, Navarro PC. Multisource, phase-controlled radiofrequency for treatment of skin laxity: Correlation between clinical and in-vivo confocal microscopy results and real-time thermal changes. J Clin Aesthet Dermatol. 2011;4:28–35.
- Harth Y, Elman M, Ackerman E, Frank I. Depressed acne scars—effective, minimal downtime treatment with a novel smooth motion non-insulated microneedle radiofrequency technology. J Cosmet Dermatol Sci App. 2014;4:212–218.
- Gold M, Taylor M, Rothaus K, Tanaka Y. Noninsulated smooth motion, microneedles RF fractional treatment for wrinkle reduction and lifting of the lower face: international study. Lasers Surg Med. 2016:48;727–733.
- Tanaka Y. Long-term nasal and peri-oral tightening by a single fractional noninsulated microneedle radiofrequency treatment. J Clin Aesthet Dermatol. 2017;10(2):45-51.
- Kaplan H, Kaplan L. Combination of microneedle radiofrequency (RF), fractional RF skin resurfacing and multi-source non-ablative skin tightening for minimal-downtime, full-face skin rejuvenation. J Cosmet Laser Ther. 2016;18(8):438–441.
- Pudukadan D. Treatment of acne scars on darker skin types using a noninsulated smooth motion, electronically controlled radiofrequency microneedles treatment system. Dermatol Surg. 2017;43:64–69.
- Park JY, Lee EG, Yoon MS, et al. The efficacy and safety of combined microneedle fractional radiofrequency and sublative fractional radiofrequency for acne scars in Asian skin. J Cosmet Dermatol. 2016;15(2):102–107
- Cho SI, Chung BY, Choi MG, et al. Evaluation of the clinical efficacy of fractional radiofrequency microneedle treatment in acne scars and large facial pores. Dermatol Surg. 2012;38:
1017–1024. - Chandrashekar BS, Sriram R, Mysore R, et al. Evaluation of microneedling fractional radiofrequency device for treatment of acne scars. J Cutan Aesthet Surg. 2014 ;7(2):93–97.
- Harth Y, Elman M, Ackerman E, Frank I. Depressed acne scars—effective, minimal downtime treatment with a novel smooth motion noninsulated microneedle radiofrequency technology. Journal of Cosmetics, Dermatological Sciences and Applications. 2014; 4:212–218.
- Graber EM, Tanzi EL, Alster TS. Side effects and complications of fractional laser photothermolysis: experience with 961 treatments. Dermatol Surg. 2008;34: 301–305.
- Tanaka Y. Long-term three-dimensional volumetric assessment of skin tightening using sharply tapered non-insulated microneedle radiofrequency applicator with novel fractionated pulse mode in Asians. Lasers Surg Med. 2015;47(8):626–633.
- Harth Y, Frank I. In vivo histological evaluation of non-insulated microneedle radiofrequency applicator with novel fractionated pulse mode. J Drugs Dermatol. 2013;12:1430–1433.
- Sadick NS, Makino Y. Selective electro-thermolysis in aesthetic medicine: a review. Lasers Surg Med. 2004;34(2):91–97.

