 by Esther RoE, PhD; Esther Serra, PhD; German Guzman, PhD; and Ignacio Sajoux, PhD
by Esther RoE, PhD; Esther Serra, PhD; German Guzman, PhD; and Ignacio Sajoux, PhD
Drs. Roe and Serra are with the Dermatology Department at the Hospital de la Santa Creu i Sant Pau in Barcelona, Spain. Drs. Guzman and Sajoux are with the Medical Department at the PronoKal Group in Barcelona, Spain.
Funding: This work was funded by a grant of Pronokal Group.
Disclosures: Drs. Roe and Serra have no conflicts of interest to relevant to the content of this article. Drs. Guzman and Sajoux are medical advisors to the PronoKal Group.
Abstract: Background: Poor eating habits, a sedentary lifestyle, and limited physical activity are predisposing factors for the development of cellulite. The PnKCelulitis® Programme (Pronokal Group, Barcelona, Spain) is a new approach to the treatment of cellulite that combines dietary guidelines, physical exercise, and the application of an anti-cellulite cream. Objective: We sought to objectively and via cutaneous ultrasound assess the benefit of the new multidisciplinary anti-cellulite treatment program and to evaluate any visual changes in the appearance of the skin. Materials and methods: Twenty women with Grades 1 to 3 cellulite were included in the study. All women underwent the multidisciplinary treatment. Clinical controls assessed the evolution of the degree of cellulite; the anthropometric parameters (e.g., weight, body mass index, and mean and low abdominal circumference) and body composition were assessed by bioimpedance. Ultrasound assessments were performed blinded at the beginning and at the end of treatment to assess the following: thickness of the skin, dermis, and hypodermis; areas of indentation; and changes in the echogenicity of the dermis. Results: The degree of cellulite was reduced in all locations, and 90 percent (18/20) of the sample saw their cellulite reduced by at least one degree. Cellulite in the abdomen disappeared in all of the women who had initially presented with it. Most of the subjects with cellulite in the buttocks (70%, 13/19) completed the treatment with Grade 0. There was a decrease in weight and a reduction of abdominal perimeters at the expense of only body fat. Significant decreases in the thickness of the skin and hypodermis and in areas of indentation were observed (p<0.05), in addition to an increase in the echogenicity of the dermis in 18 of the 20 patients. Conclusions: The multidisciplinary treatment program evaluated in this study appears to be an effective and safe treatment for patients with different degrees of cellulite, both clinically and via ultrasound imaging. Additional research with a larger patient cohort is needed to support our findings.
Keywords: Cellulite, ultrasonography, adipose tissue , therapeutics, PnKCelulitis®
J Clin Aesthet Dermatol. 2018;11(3):20–25
Cellulite, or edematofibrosclerotic panniculopathy, is a cutaneous disorder that involves a disruption of the subcutaneous fat tissue, causing alteration of the body shape and affecting the appearance of the skin. It is accompanied by changes in the microcirculation of the connective tissue, which provoke morphological, histochemical, and biochemical modifications in the tissue. The disorder is characterized by a padded and nodular appearance of the skin in declining areas. It is a disorder that affects 85 to 98 percent of female individuals after puberty and is considered to be a secondary sexual trait in women.1,2
Regarding multifactorial etiology, the pathophysiology of cellulite is complex and includes expansion of subcutaneous fat, formation of fibrotic septa in the dermis, dermal laxity, and atrophy.3 Direct effects of hormonal changes, genetic factors, family tendencies to abnormal fat deposition, and poorly developed muscle mass all predispose people to the development of cellulite.
Poor eating and lifestyle habits are also predisposing factors for the development of cellulite. An unbalanced diet, especially with increased consumption of carbohydrates and fats, leads to a state of hyperinsulinemia that, among other effects, intensifies the process of lipogenesis and increases fat tissue. The consumption of processed foods with large amounts of preservatives or high levels of salt intake increases fluid retention and edema.4 Additionally, poor physical activity/sedentary lifestyle also contribute to the development of this cutaneous disorder as they affect microcirculation and favor the accumulation of fat.4
A wide variety of noninvasive treatments have been proposed for the treatment of cellulite, from weight loss (the most frequent) to treatments with massages and the use of topical agents (creams), shockwave treatments, and oral supplements. Massages, whether by hand or mechanical in nature, such as lipomassage (e.g., Endermologie®, LPG Endermologie, United Kingdom) improve venous return and reduce edema. There is also some evidence that the tensional forces exerted on the extracellular matrix stimulate the synthesis of collagen by fibroblasts and decrease activity and differentiation of the adipocytes, which could explain the beneficial effects of massage on the signs of cellulite.5,6 Topical creams contain different types of agents, such as xanthines, botanicals, fragrances and ligands of the retinoid, and peroxisome proliferator-activated receptors (PPARs), which, through the reduction of adipogenesis and the increase of thermogenesis, appear to improve microcirculation and collagen synthesis. In addition, the application of creams also involves a massage, which could contribute to their benefits.2
The use of high-energy radiofrequency waves act by increasing the temperature of the deep skin, which causes the skin collagen fibers to contract, in addition to reducing fat when used repeatedly.7 Use of high-energy radiofrequency waves can assist in improving the volume and structure of the skin and the appearance of cellulite in 50 percent of cases.8,9 Shock waves, meanwhile, can physically impact the tissues by restructuring skin properties and subcutaneous tissue, thus clinically improving aspects of cellulite and localized fat.10 In addition, many oral weight-management supplements (e.g., hydroxycitrate, epigallocatechin gallate, conjugated linoleic acid [CLA]) are being studied for their effects on cellulite; in particular, CLA has been shown to improve the signs of cellulite. Regular exercise and a healthy diet can also help control weight and thus improve the appearance of cellulite.2
The PnKCelulitis® Programme (Pronokal Group, Barcelona, Spain) is a new multidisciplinary approach to the treatment of cellulite that includes dietary guidelines, physical exercise, and the topical application of a cream. The dietary pattern includes a hypocaloric diet and protein supplements. The diet, which in the first few weeks is ketogenic with a very restricted supply of carbohydrates, is able to increase lipolysis and reduce fat tissue while also improving the drainage of liquids. The supply of protein supplements along with physical exercise should increase muscle mass and reverse underlying sagging while improving microcirculation and mobilizing fat deposits. The treatment is complemented by the application of a cosmetic cream to assist in reducing lipogenesis and improving circulation.11
The objective of this study was to evaluate the benefits of the above described multidisciplinary treatment program for cellulite, objectifying it through the changes observed in the structure of the dermis and the subcutaneous tissue by cutaneous ultrasound,12 as well as assess changes in the visual appearance of the skin in the affected areas.
Materials and methodology
This clinical trial was exploratory, prospective, uncontrolled, and single-blinded, with clinical and ultrasound assessments of cutaneous cellulite before and after treatment. The participants underwent a specific multidisciplinary program that included dietary guidelines, physical exercise, and the application of a cosmetic cream. The program was carried out in the dermatology department of the Santa Creu i Sant Pau Hospital in Barcelona, Spain, and in collaboration with medical consultations held at the Pronokal Group premises in Barcelona. The study was evaluated and approved by the Clinical Research Ethics Committee of the Santa Creu i Sant Pau Hospital; all participants were informed of the objectives of the study and signed an informed consent form with respect to their participation and for photographs being taken.
Patients. Women older than 18 years of age of normal weight and with cutaneous non-infectious cellulite (edematous-fibrosclerotic panniculopathy) were recruited for the study. Exclusion criteria were the same as those that are established by the multidisciplinary treatment due to contraindications of a ketogenic diet, and included pregnant or lactating women; patients with eating disorders, alcoholism, and/or drug addiction; patients with severe psychological disturbance (e.g., schizophrenia, bipolar disorder, depression); patients being treated with dicoumarinic anticoagulants (acenocoumarol) or cortisone; and patients with hepatic insufficiency, severe renal insufficiency (glomerular filtration rate <30), Type 1 or Type 2 diabetes mellitus, insulin dependency, hemopathies, cancer, cardiovascular or cerebrovascular diseases, acute gout attack, renal lithiasis confirmed by ultrasound, cholelithiasis confirmed by ultrasound, electrolytic disorders, medical criteria, or orthostatic hypotension.
Treatment. All participants were treated with the multidisciplinary program (Table 1), which consisted of three phases: 1) restructuring, 2) drainage, and 3) toning, each of which combines diet, physical exercise, and the application of an anti-cellulite cream (Cellulite Gel K-Line®, PronoKal Group, Barcelona, Spain), which was a gel-like cosmetic product comprising coralline officinalis, caffeine, L-carnitine, resveratrol, and phosphatidylcholine. The dietary phase began with a ketogenic low-calorie diet (800–1,200kcal/day) based on high-biological-value protein preparations which contained 15g protein, 4g carbohydrates, 3g fat, and 50mg docosahexaenoic acid and supplements of vitamins and minerals. The diet was then modified to a non-ketogenic low-calorie diet (1,200–1,500kcal/day), accompanied by two protein products, , one at mid-morning and one at mid-afternoon, until end of study. Physical activity phase comprised toning exercises that progressively increased in difficulty and intensity. After physical exercise, the patients took an extra protein product and applied the anti-cellulite cream to the affected areas, lightly massaging the cream into the target areas until totally absorbed.
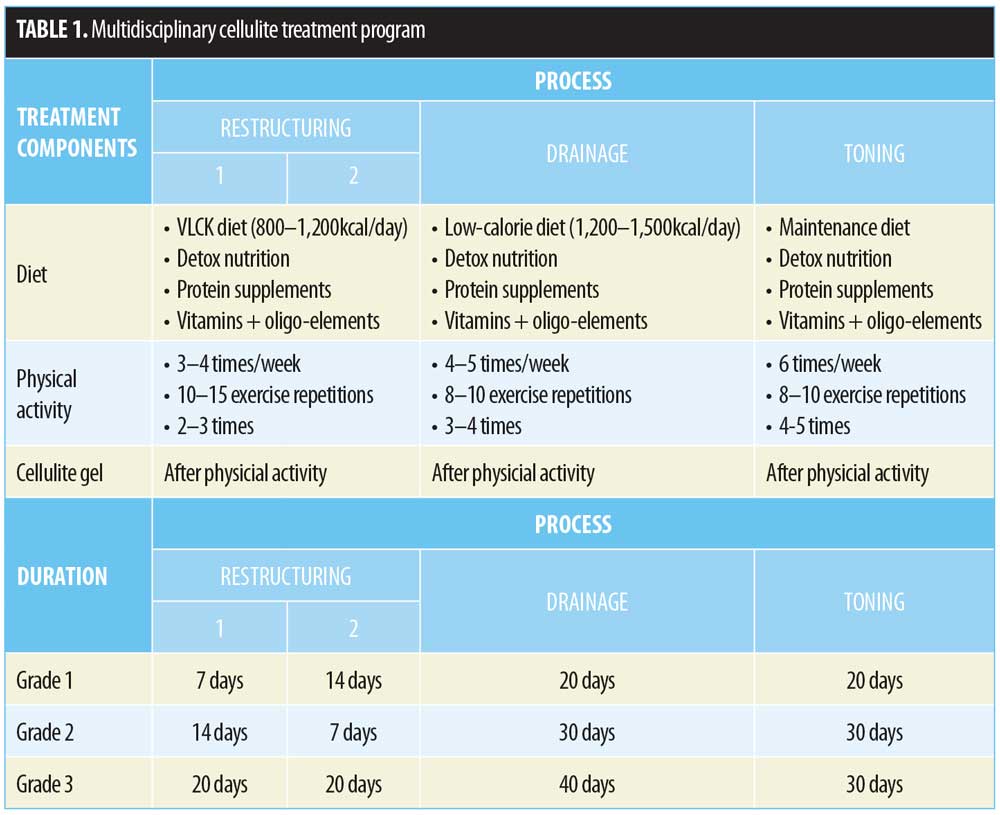
The duration of the ketogenic diet before converting to the non-ketogenic diet, as well as the multidisciplinary program as a whole were set according to each patient’s initial amount of cellulite. Thus, for patients with Grade 1 cellulite, the expected duration of treatment was 61 days, with 21 days on the ketogenic diet and 40 days on the non-ketogenic diet. For patients with Grade 2 cellulite, the expected duration was 81 days (21 days ketogenic diet, and 60 days non-ketogenic diet). For patients with Grade 3 cellulite, the expected duration was 110 days (40 days ketogenic, 70 days non-ketogenic diet).
Clinical assessments. Patients’ clinical assessment follow-ups were performed by the prescribing doctor of the multidisciplinary treatment and were done in four visits occurring at baseline (before starting treatment) and at the end of each of the restructuring, drainage, and toning phases, respectively. Anthropometric data were recorded at each visit and included weight, body mass index (BMI), mean abdominal perimeter (navel level), low abdominal perimeter (5cm below the navel), thigh perimeter, and results from a bioelectric impedance test to assess body composition (amount of fat mass and muscle mass).
The clinical evaluation of the degree of cellulite was made according to the Nürnberger–Muller classification scale (Grade 0: no dimples; Grade 1: dimples are observed only upon application of the pinch test; Grade 2: dimples appear with standing but not lying down; and Grade 3: there is spontaneous presence of dimples with standing or lying down). Photographs were taken of the gluteal (posterior) and hips (right and left profile) of each participant at each visit, with the patient standing upright, at a distance of 50cm using a tripod, with a focus from the iliac crest to the knee, always in the same place, and under the same lighting conditions.
Ultrasound evaluations. Cutaneous ultrasound was performed by an expert dermatologist in the dermatology outpatient clinic of the hospital and subsequently assessed in a blinded manner (i.e., two skin scans were done for each patient—one prior to the start of the treatment and another at the end—and were blinded and assessed by two researchers). Ultrasounds were performed on the left thigh on the midpoint between the iliac crest and the head of the fibula, with the performance of the measurement done with a tape measure. The objective data collected on each ultrasound were total skin thickness, thickness of the dermis and hypodermis, and the area of the indentations of the subcutaneous cellular tissue in the dermis. The largest indentation was chosen by ultrasound scanning of the explored area. To measure the thickness of the different layers of the skin, 18MHz frequency imaging probe was used, and two 22MHz frequency imaging probes were employed to assess the dermis and indentations.
The changes in the echogenicity of the dermis from the images of the ultrasound were also blinded and independently assessed by two researchers, who compared ultrasounds before and after treatment. The blinded interpretation was based on a 3-point scale: 1=increased echogenicity (improvement); 0=unchanged (same); and -1=decreased (worsening echogenicity).
Statistical analysis. The baseline demographic, clinical, and ultrasound data were presented using descriptive statistics, mean±standard deviations (SDs), and medians and quantitative variables and employed frequencies (n) and percentages (%) for qualitative or ordinal variables.
For the main objectives, the clinical and ultrasound evaluations were compared between visits by means of the chi-squared (?2) test in the case of qualitative variables and the Student’s t-test for paired data in the case of quantitative variables.
The data were analyzed using the statistical software SAS, version 9.1.3 Service Pack 4 (SAS Institute, Cary, North Carolina, USA). For all tests, the level of statistical significance was set at p<0.05.
Results
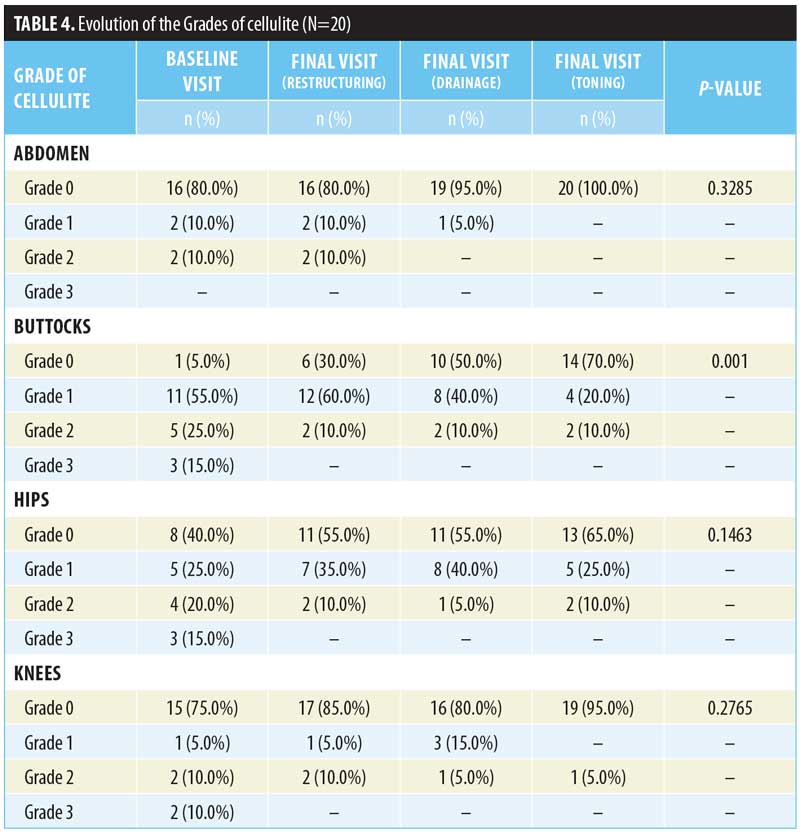
A total of 20 female participants aged 29 to 58 years (mean: 41.25±9.37 years) with cutaneous cellulite were treated with the multidisciplinary program. Fifty percent (n=10) presented with Cellulite Grade 1, 35 percent (n=7) presented with Cellulite Grade 2, and 15 percent (n=3) presented with Cellulite Grade 3. The most frequent location of the cellulite was in the buttocks (95.0%), followed by the hips (60.0%), knees (25.0%), and abdomen (20.0%) (Table 2).
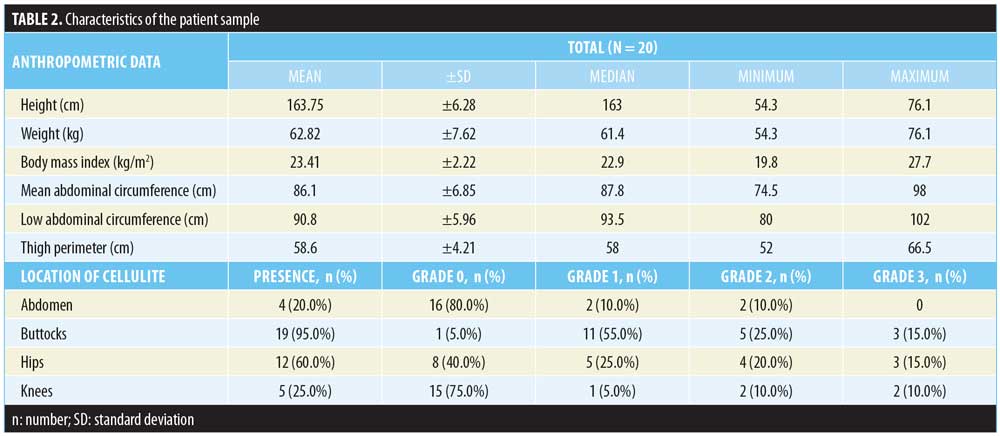
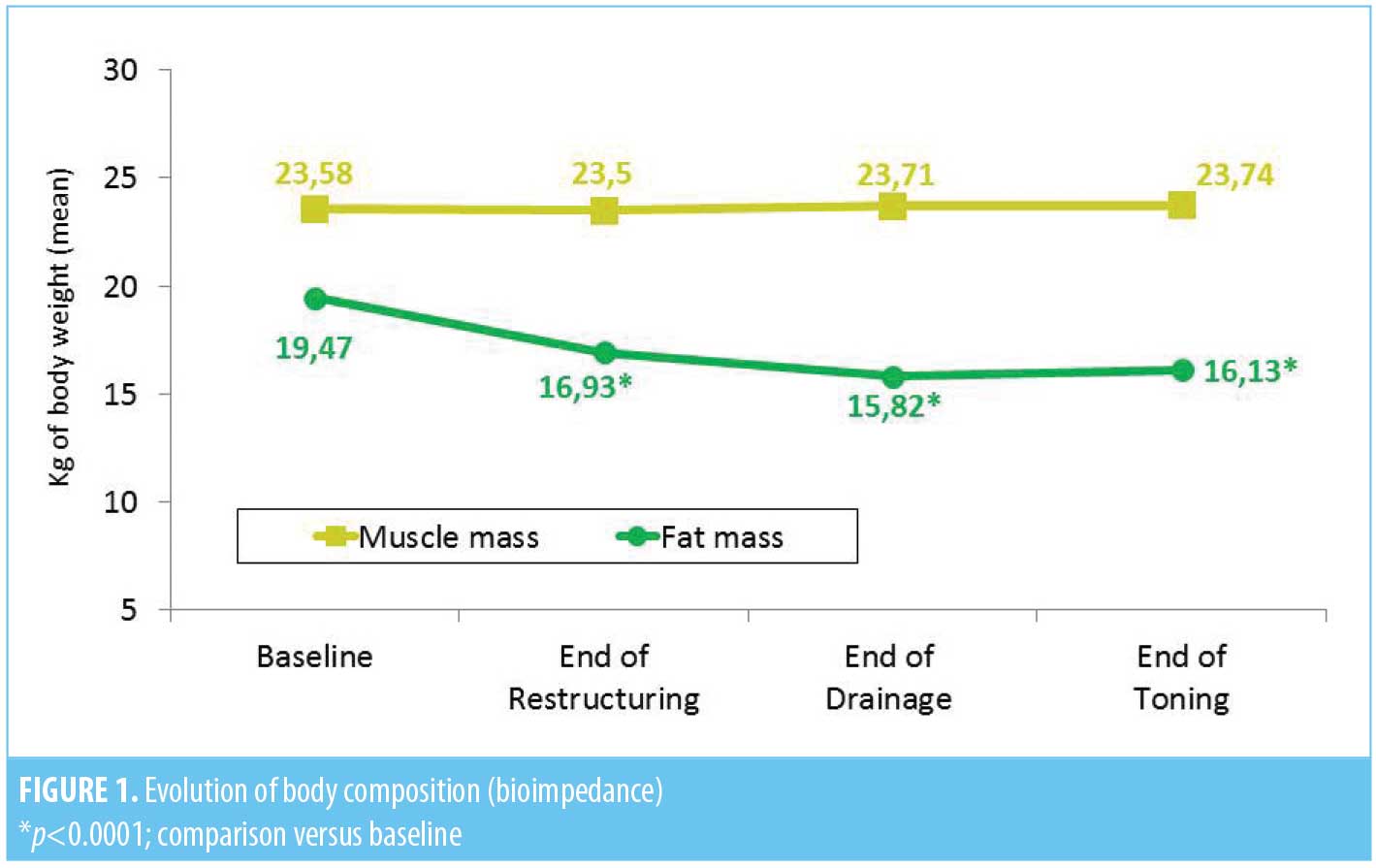
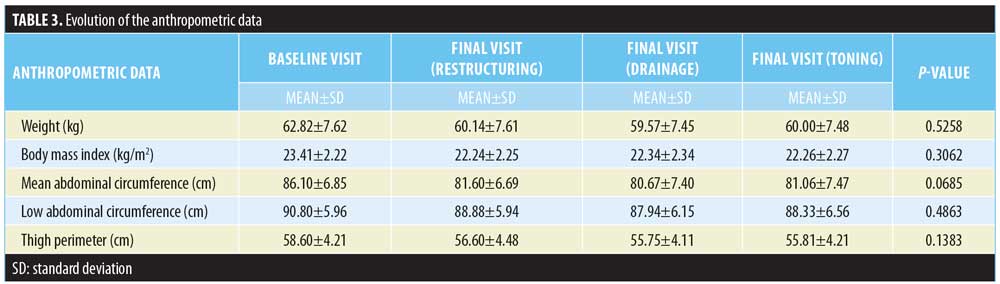
Clinical parameters. At the end of the treatment, the women presented a discrete but significant (p<0.0001) weight and BMI loss at the expense of body fat loss. Thus, while skeletal muscle mass remained unchanged (23.58±2.4kg vs. 23.74±2.62kg, p=0.9899), the amount of fat decreased significantly (19.47±5.46kg vs. 16.13±5.23kg, p<0.0001) (Figure 1). This weight loss was accompanied by a decrease in mean abdominal circumference (86.10±6.85cm vs. 81.06±7.47cm, p<0.0001); low abdominal perimeter (90.80±5.96cm vs. 88.33±6.856cm, p<0.0005); and thigh perimeter (58.60±4.21cm vs. 55.81±4.21cm, p<0.0001) (Table 3).
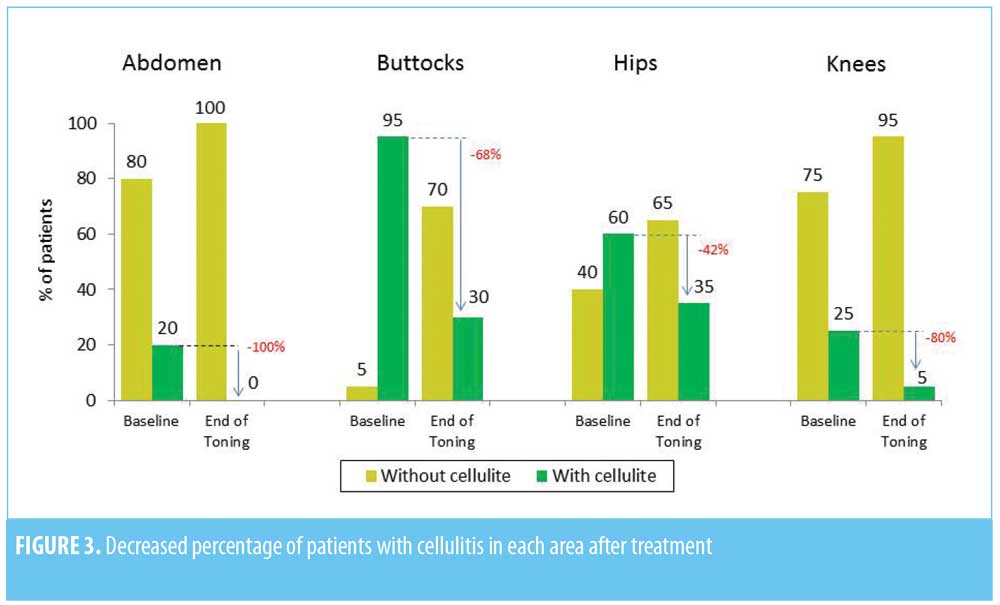
The degree of cutaneous cellulite assessed by the prescribing doctor decreased in all locations (Figure 2) and was statistically significant (p<0.05) at the gluteal level (Table 4). The degree of cellulite for 90 percent (n=18) of the participants decreased by at least one grade. The cellulite located in the abdomen, which affected 20 percent (n=4) of the participants, disappeared in all cases. In the buttocks and hips, Grade 2 and Grade 3 cellulite, present in 40 percent (n=8) of the participants at the beginning of the study, dropped to being present in only 10 percent (2=20) of the participants. While of the remaining 90 percent, 18 of 20 participants finished the treatment without cellulite (Grade 0) on their gluteal (70%, 13/19) and/or hip (65%) areas. Of the 25 percent (n=5) of participants with knee cellulite, only one subject had cellulite at this location at the end of treatment (Figure 3).

Ultrasound parameters. The multidisciplinary treatment resulted in a significant decrease in total skin thickness (31.38±11.30mm vs. 22.74±8.52mm, p=0.0096) that occurred mainly at the expense of a decrease in the thickness of the skin hypodermis (29.53±11.00mm vs. 20.76±8.23mm, p=0.0069). Conversely, the dermis did not show significant changes (1.49±0.34mm vs. 1.57±0.27mm, p=0.4385), showing a nonstatistically significant tendency to increase. There were also significant changes in indentation areas that decreased from a mean of 0.03cm2 to 0.02cm2 (p=0.0074). Likewise, an improvement in the quality of the dermohypodermic junction and an increase in the echogenicity of the dermis were observed in 18 of the 20 participants. No change or signs of deterioration were observed in two patients. The inter-rater correlation of echogenicity assessments was 100 percent.
Tolerability data and overall treatment assessment. Treatment was well-tolerated. Only mild and transient side effects were reported, with abdominal discomfort and constipation being the most frequent ones seen in the first days of the ketogenic diet.
Discussion
The results of this study suggest that the multidisciplinary treatment program is effective in significantly improving the degree of cellulite in the buttocks and hips and in reducing edema, thickness, and areas of indentation at the dermis and hypodermis levels. This was accompanied by a decrease in body measurements and weight at the expense of adipose tissue alone, without loss of muscle mass.
Treatment for cellulite has not been well-established. Studies on other therapies have not yet demonstrated strong, long lasting results.14 Given the implication of multiple factors (i.e., genetic, hormonal, sedentary lifestyles, eating habits) and the pathophysiology of cellulite, a treatment that targets these multiple factors would be of value. The multidisciplinary treatment program that was assessed in this study resulted in positive effects on the appearance of cellulite; Additionally, this treatment approach might also help individuals acquire healthier eating and lifestyle habits that might help prolong it effects and prevent the reappearance of cellulite.
All 20 participants showed an improvement in the degree of cellulite they had, as well as a decrease in body weight and circumference measurements for the medium and low abdominal and thigh areas. Unlike other dietary approaches to improving cellulite, the combination of a ketogenic diet, protein intake, and exercise allowed the participants to lose fat without losing muscle mass.
Sedentary lifestyle and lack of physical activity are usually accompanied by muscular hypotonicity, which can slow blood and lymphatic microcirculation, causing edema in declining areas such as the buttocks. Physical activity and a high-protein diet can contribute to strengthening muscle and improving circulation and lymphatic drainage of areas with cellulite.
The reduction of the fat tissue observed in our participants was likely mainly due to the low-fat ketogenic diet, in which the restriction of carbohydrates led to physiological ketosis, where the body had to obtain energy from the fatty acids released by adipose tissue through a lipolysis process. This lipolytic effect of the diet was boosted by the application of an anti-cellulite cream, which comprised caffeine (with proven lipolytic effects and lymphatic circulation stimulant15); L-carnitine (responsible for transporting fatty acids to the mitochondria for ?-oxidation and producing energy16); and phosphatidylcholine (which stimulates the hydrolysis of triglycerides in the adipocytes17), in addition to other substances that also act on the cells of fat tissue.
Objectively assessing the effectiveness of any cellulite treatment is difficult. Our study recorded objective results of the treatment through cutaneous ultrasound. The introduction of high-frequency ultrasound (>18MHz) in dermatology and aesthetic medicine provides us with an inexpensive, noninvasive, safe, and objective tool for evaluating the dermis and the subcutaneous cellular tissue of our patients with great precision; thus, ultrasound assessment can be a very useful tool in monitoring cellulite treatments.
Previous studies2,6 have shown that the most useful parameters for evaluating cellulite with ultrasound are the subcutaneous cellular tissue (SCT) thickness, the size of the SCT indentations in the dermis, and the echogenicity of the dermis. In agreement with the study published by Mlosek et al,12 our participants showed statistically significant reductions of the SCT thickness and the areas and perimeters of the SCT indentations in the dermis. An increase in the echogenicity of the dermis and a better visual aspect of the union of the dermis and the SCT were also observed at the end of the study. The thickness of the dermis in cellulite and its variation with treatments is controversial. There are studies that did not find variations between dermal thickness in patients with or without cellulite,8 while other studies have reported decreases in dermal thickness and dermal density in patients with cellulite.9 The study carried out with ultrasound control by Mlosek et al12 found a dermal reduction, probably due to a decrease in edema. In our sample, we did not observe a significant variation, but there was a nonstatistically significant tendency of increased thickness that suggests an increase in echogenicity of this tissue and an increase in the production of collagen.
Limitations. A limitation of the study is the lack of a control group. However, as there is no gold standard treatment for cellulite we could use for comparison, the participants at baseline were used as controls. Another limitation was our inability to determine and quantify how much of the cellulite reduction was due to each of the individual components of the treatment regimen (i.e., diet, exercise, or anti-cellulite cream). However, the treatment program is designed to counteract the underlying changes of cellulite (e.g., subcutaneous fat), by causing structural changes such as weight loss, reduction in edema, and improvement in hypotonicity and microcirculation. Therefore, testing each component separately would be at odds with the overall mechanisms of the treatment program.
The grading scale we used in our study is not the typical one recommended for cellulite evaluation. For this study, we decided to use two rating scales to assess the degree of cellulite: a simple, direct, and immediate evaluation by the physician, feasible for use in the doctor’s office, and another, more complex scale based on photographic images (the Hexsel Photonumeric Cellulite Severity Scale) that were blindly assessed a posteriori by two independent evaluators. This article describes the ultrasonographic and clinical changes in cellulitis based on physician assessment. The Hexsel Photonumeric Scale, and its statistical analysis, for the clinical evaluation of cellulitis via photographic images is still under evaluation, and the results of its assessment will be the object of another publication.
Conclusion
The multidisciplinary treatment program (PnKCelulitis®; PronoKal Group, Barcelona, Spain) assessed in this study is a new approach to the treatment of cellulite. Results of our study suggest that this treatment program is safe and effective in improving different degrees of cellulite, as measured clinically and by ultrasound. Additional research with a larger sample size is needed to support our findings regarding the safety and effectiveness of the treatment program. However, based on our study and those previously reported in the literature, we conclude that high frequency ultrasound is a useful tool for evaluating and monitoring cellulite during treatment.
References
- Khan MH, Victor F, Rao B, Sadick NS. Treatment of cellulite: part I. Pathophysiology. J Am Acad Dermatol. 2010;62(3):361–370.
- Rawlings AV. Cellulite and its treatment. Int J Cos Sci. 2006;28(3):175–190.
- Rossi AM, Katz BE. A modern approach to the treatment of cellulite. Dermatol Clin. 2014;32(1):51–59.
- Leszko M. Cellulite in menopause. Prz Menopauzalny. 2014;13(5):298–304.
- Adcock D, Paulsen S, Jabour K, et al. Analysis of the effects of deep mechanical massage in the porcine model. Plast Reconstr Surg. 2001;108(1):233–240.
- Tanabe Y, Koga M, Saito M, et al. Inhibition of adipocyte differentiation by mechanical stretching through ERK-mediated downregulation of PPARgamma2. J Cell Sci. 2004;117(Pt 16):3605–3614.
- Alizadeh Z, Halabchi F, Mazaheri R, et al. Review of the mechanisms and effects of noninvasive body contouring devices on cellulite and subcutaneous fat. Int J Endocrinol Metab. 2016;14(4):e36727.
- Manuskiatti W, Wachirakaphan C, Lektrakul N, Varothai S. Circumference reduction and cellulite treatment with a TriPollar radiofrequency device: a pilot study. J Eur Acad Dermatol Venereol. 2009;23(7):820–827.
- Emilia del Pino M, Rosado RH, Azuela A, et al. Effect of controlled volumetric tissue heating with radiofrequency on cellulite and the subcutaneous tissue of the buttocks and thighs. J Drugs Dermatol. 2006;5(8):714–722.
- Modena DAO, da Silva CN, Grecco C, et al. Extracorporeal shockwave: mechanisms of action and physiological aspects for cellulite, body shaping, and localized fat–systematic review. J Cosmet Laser Ther. 2017;19(6):314–319.
- Pronokal Group. Programa PnKCelulitis. http://www.pronokalgroup.com/es/pnkcelulitis/. Accessed January 27, 2018.
- Mlosek RK, D?bowska RM, Lewandowski M, et al. Imaging of the skin and subcutaneous tissue using classical and high-frequency ultrasonographies in anti-cellulite therapy. Skin Res Technol. 2011;17(4):461–468.
- Nürnberger F, Müller G. So-called cellulite: an invented disease. J Dermatol Surg Oncol. 1978;4(3): 221–229.
- van der Lugt C, Romero C, Ancona D. et al. A multicenter study of cellulite treatment with a variable emission radio frequency system. Dermatol Ther. 2009;22(1):74–84.
- Herman A, Herman AP. Caffeine’s mechanisms of action and its cosmetic use. Skin Pharmacol Physiol. 2013;26(1):8–14.
- Vaz FM, Wanders RJ. Carnitine biosynthesis in mammals. Biochem J. 2002;361(Pt 3):417–429.
- Sasaki GH, Oberg K, Tucker B, Gaston M. The effectiveness and safety of topical PhotoActif phosphatidylcholine-based anti-cellulite gel and LED (red and near-infrared) light on Grade II-III thigh cellulite: a randomized, double-blinded study. J Cosmet Laser Ther. 2007;9(2):87–96.
- Querleux B, Cornillon C, Jolivet O, Bittoun J. Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: relationships with sex and presence of cellulite. Skin Res Technol. 2002;8(2):118–124.
- Ortonne JP, Zartarian M, Verschoore M, et al. Cellulite and skin ageing: is there any interaction?. J Eur Acad Dermatol Venereol. 2008;22(7):827–834.

