 by Philip R. Cohen, MD, and S. Brian Jiang, MD
by Philip R. Cohen, MD, and S. Brian Jiang, MD
Drs. Cohen and Jiang are with the Department of Dermatology at the University of California San Diego, in La Jolla, California.
J Clin Aesthet Dermatol. 2017;10(8):42–48
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the contents of this article.
Keywords: Carcinoma, cell, digit, distal, finger, pad, palmar, squamous, ventral
Abstract: Background. Squamous cell carcinoma of the palmar digits is rare. Purpose: The authors describe a man with squamous cell carcinoma of the pulp of his left fourth finger, and review the risk factors that may be associated with squamous cell carcinoma development on the ventral digits of the hand. The authors also summarize the clinical differential diagnoses and treatment of squamous cell carcinoma at this location.
Methods. The authors retrospectively reviewed the literature using PubMed and searched for the following terms: squamous cell carcinoma, squamous cell carcinoma in situ, finger, thumb, palmar, and ventral. Papers were critically evaluated and their cited references reviewed.
Results. Skin biopsy established the patient’s diagnosis. His tumor was excised using Mohs technique with microscopic examination of the tissue margins; viral changes were noted in the keratinocytes. Local or systemic carcinogen exposure, congenital conditions, suppressed host immunity, coincidental bacterial or viral infection, local radiation exposure, and trauma to the affected digit are risk factors associated with the development of palmar digit squamous cell carcinoma. The clinical differential diagnoses of squamous cell carcinoma on the ventral digits include chronic dermatitis and keratoderma, epidermoid cyst, infection, melanoma, and verrucae. Successful treatment involves removal of the tumor; this is usually accomplished by surgical excision of the tumor, which may include some or all of the affected digit.
Conclusions. The diagnosis of squamous cell carcinoma of the ventral hand digits is often not initially suspected by the patient and/or the clinician. However, despite the occasional delay in diagnosis or subsequent large tumor size, the prognosis for these patients is usually favorable following adequate treatment of the cancer.
Introduction
Cutaneous squamous cell carcinoma (SCC) is a nonmelanoma skin cancer (NMSC) that typically occurs on sun-exposed skin. In contrast, SCC and SCC in situ of the palmar aspect of the hand digits are rare. A man with SCC of the distal pad of his left fourth finger is described and features associated with SCC of the ventral finger are reviewed.
Case Report
A 62-year-old, Fitzpatrick type I, Caucasian man presented with a mass on the palmar aspect of his left fourth finger pulp. The lesion had been originally noted five years earlier and
interpreted by the patient to be a wart. It progressively enlarged in size and was often painful.
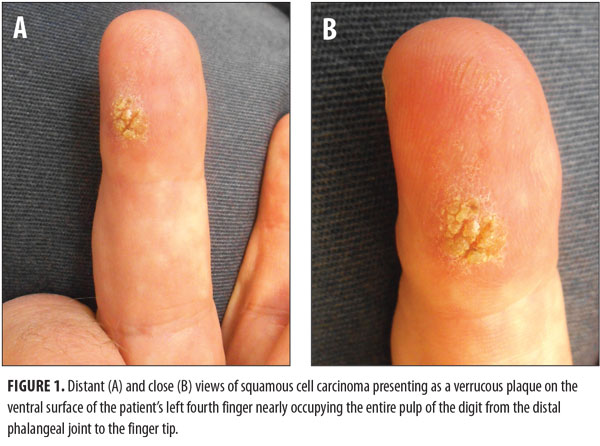
Cutaneous examination showed a 20mm x 15mm verrucous plaque that nearly occupied the entire ventral surface of the left fourth finger from the distal interphalangeal joint to the tip of the finger (Figure 1). There was no axillary lymphadenopathy. A 3mm punch biopsy was performed, and the histopathology showed SCC, with invasion of atypical keratinizing epithelium into the underlying dermis.
The residual cancer (Figure 2) was removed by Mohs surgery using the frozen-tissue
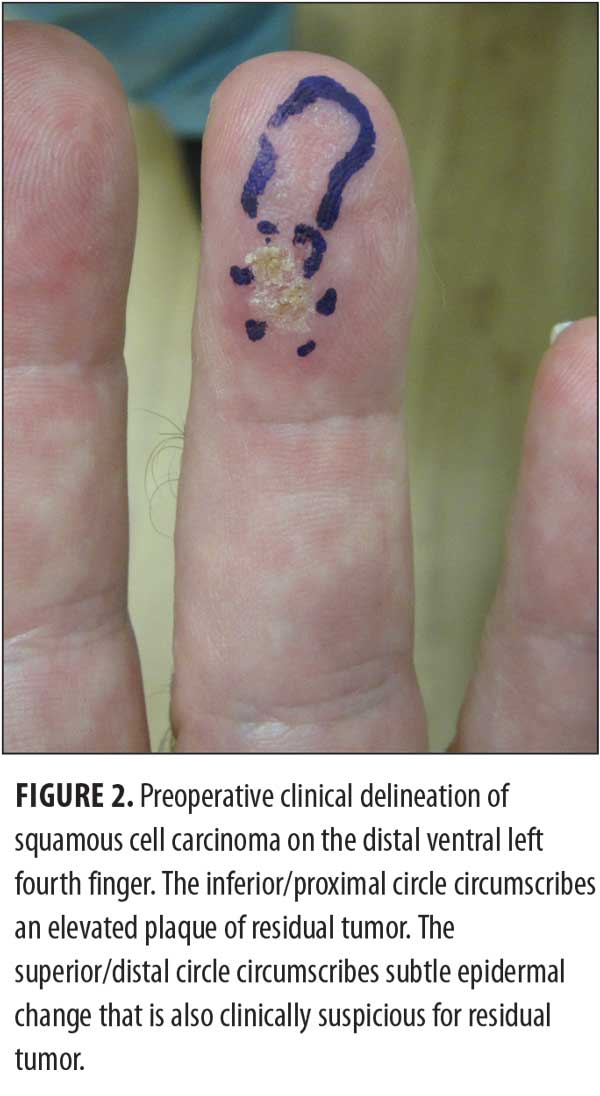
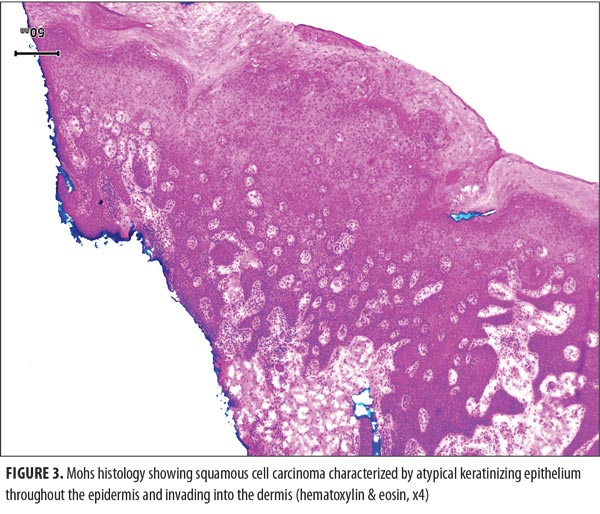
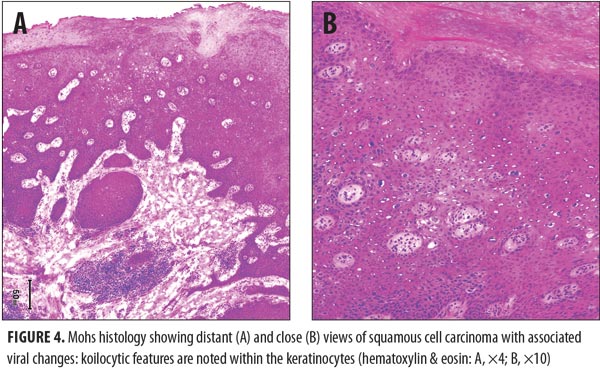
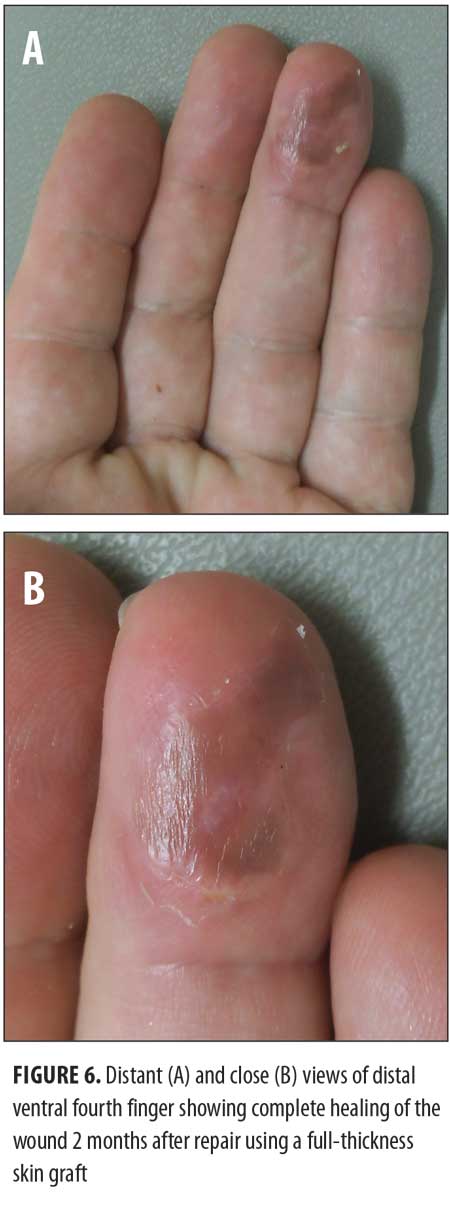
technique. Five stages were required to clear the tumor. Microscopic review of the surgical specimen not only showed full-thickness keratinocyte atypia within the epidermis with islands of atypical squamous cells invading the dermis (Figure 3) but also cytologic features consistent with human papillomavirus (HPV) changes within the keratinocytes (Figure 4).The resulting wound (Figure 5) was repaired using a full-thickness skin graft derived from the left lower quadrant of his abdomen. The donor and recipient sites healed without any complications. His follow-up physical examination two months later showed no evidence of tumor (Figure 6).

Discussion
SCC of the ventral fingers. SCC of the dorsal hand is common. In contrast, periungual and distal dorsal finger SCC—often associated with HPV—is onlyoccasionally observed.[1–4] SCC on the nonsun-exposed ventral fingers is rare.
Risk factors for SCC of the ventral fingers. Previously documented risk factors for SCC include arsenic ingestion, chronic scars, chronic ulcers, HPV infection, radiation therapy, reduced immunity, trauma, and ultraviolet light (e.g., sun) exposure.[5–7] With the exception of sun exposure (which is unlikely to chronically occur to the palmar surface of the fingers), these and other risk factors have been observed in individuals with SCC of the ventral fingers (Table 1).[6–26]
Carcinogen exposure. Exposure to carcinogens can result in malignancy. Palmar digit SCC occurred in individuals exposed to arsenic, grease and oil, or “soluble oil.”[6–9] A 49-year-old man with psoriasis and a long history of exposure to arsenic from herbal medicines developed an SCC in situ on his distal palmar right fifth finger.[7] Another individual with chronic arsenism, a 74-year-old Taiwanese man, also developed an SCC on the distal pad of his right index finger.[6]
Exposure to oil contributed to SCC developing on the ventral left thumb of a 59-year-old truck mechanic with extensive contact with grease and oil and recurrent episodes of trauma to the digit.[8] Soluble-oil metalworking fluids, which contain emulsified naphthenic or paraffinic oils in water, are used for cooling and lubrication of cutting tools and the working surface. A 77-year-old man, who was employed for 50 years as a metal lathe turner working with soluble oil, developed SCCs of both ventral thumbs and five palmar digits.[9]
Congenital condition. Epidermolysis bullosa, Huriez syndrome, and syndactyly are congenital conditions that have been associated with the subsequent development of palmar digit SCC in adulthood. Recessive dystrophic epidermolysis bullosa is a rare heritable blistering disorder characterized by subepidermal blisters that often involve the fingers and the potential for skin cancer to develop in the chronic scar tissue. A 51-year-old woman with non-Hallopeau-Siemens recessive dystrophic epidermolysis bullosa developed an SCC involving both the ventral and dorsal surfaces of her right fourth finger.[10] SCCs also occurred in identical twins with recessive epidermolysis bullosa.[11]
Huriez syndrome is a rare autosomal dominant genodermatosis characterized by congenital scleroatrophy of the palms and soles, palmoplantar keratoderma, and nail changes; nonfamilial patients with Huriez syndrome have also been reported.[12,13] A 31-year-old Japanese woman with nonfamilial Huriez syndrome and palmoplantar keratoderma since birth developed an SCC on her left palmar thumb and SCC in situ on her right palmar thumb.[13] In addition, a 27-year-old Indian man with nonfamilial Huriez syndrome developed an SCC on the palmar surface of his left thumb.[12]
Syndactyly, the most common congenital abnormality of the hand, is classified as a failure of differentiation. An 81-year-old man with bilateral incomplete simple syndactyly involving the web space between his third and fourth fingers on both hands presented with verrucous SCCs affecting both the left and right palmar web spaces.[14]
Immunosuppressed host. A suppressed immune system is a risk factor for the development of NMSCs. Immunosuppression may be congenital or acquired; the latter can be associated with infection (such as human immunodeficiency virus [HIV]) or iatrogenic (following organ transplant). A cardiac transplant patient developed SCC in situ of the finger and bowenoid papulosis of the perianal area. HPV Type 16 was detected from both the tumor and the perianal lesion. The investigators hypothesized contact transmission of the viral-associated cancer of the finger.[15]
Infection. Chronic bacterial or viral infection has also been observed to precede the development of ventral digit SCC. Recurrent bacterial infections preceded the eventual diagnosis of SCC in a 60-year-old man following wood splinter injury to his left palmar thumb16 and in a 33-year-old man who sustained a small wound to the ventral aspect of his right index finger while working with wet concrete without gloves.[17]
Our patient’s SCC demonstrated viral changes and is therefore likely to be associated with a preceding HPV infection. Other cases of men with palmar digit SCC in situ have been reported; many of these individuals (or their sexual partners) also had genital SCC in situ associated with the same HPV type.[15,18,19] In addition, women with subungual and/or dorsal finger HPV associated SCC in situ have been described to also have genital dysplasia secondary to the same virus.[1,27,28]
A 60-year-old man with a hypertrophic scaling plaque on his volar and medial finger was documented to have HPV Type 16, by in-situ deoxyribonucleic acid (DNA) hybridization, in the SCC in situ from both his digit and penis.19 HPV Type 16 was also confirmed by in-situ hybridization and polymerase chain reaction in the SCC in situ of the finger and the bowenoid papulosis of the perianal area of a cardiac transplant patient.[15] Excisional biopsy of a presumed recurrent wart on a nondominant finger of a 33-year-old man showed HPV Type 16-associated SCC in situ; additional history revealed that his female partner previously had viral-related cervical lesions.[18]
Radiation exposure. SCC of the palmar finger has been observed in patients exposed to radiation.[7,20–23] This includes not only exposure to radiopharmaceuticals and ionizing radiation but also exposure to ultraviolet A radiation:
- A nurse who worked for five years in a metabolic radiotherapy unit preparing the injectable substances (e.g., thallium and metastable technetium 99) and administering radioactive tablets for thyroid tumor therapy developed an SCC in situ on the right proximal palmar third finger five years later;[20]
- A 75-year-old woman who worked for more than 30 years as an X-ray technologist holding newborns during radiological studies developed an SCC on the flexor surface of her right middle finger 15 years after retiring;[23]
- A 63-year-old pediatrician who used radioscopy for 20 years in his practice and handled children without the protection of lead gloves, presented with a radiation-associated SCC in situ in addition to biopsy-confirmed chronic radiodermatitis of the distal palmar right middle finger;[21]
- A 49-year-old man with arsenic exposure whose psoriasis had been treated with psoralen and ultraviolet A radiation developed SCC in situ of his distal palmar right fifth finger.[7]
Trauma. Severe, repetitive, and/or chronic trauma to the affected digit has been observed in some of the individuals who subsequently developed SCC of the ventral surface of that digit.[14,16,17,24–26] The development of cancer at these sites of trauma is likely similar to the occurrence of cutaneous SCC observed in chronic scars, ulcers (Marjolin ulcers), or sinuses following trauma to the skin site. Chronic irritation to the affected area is postulated to promote malignant transformation.
The latency period between the initial injury and subsequent diagnosis of cancer in patients with Marjolin ulcers or similar injuries is typically long—often ranging from 20 to 30 years.[16,17,24] In contrast, the latency period between injury and cancer detection was shorter in five of the six patients with trauma-associated SCC of the ventral finger ranging from six months to 12 years (median=10 years).[16,17,24–26] However, in an 81-year-old man with congenital syndactyly and chronic skin changes as a result of friction, the latency period was over eight decades.[14] SCC of the pulp space of the left index finger developed in a roofer following repeat hammer blows to the same finger six months and 12 years earlier.[25] In addition, squamous cell carcinomas have subsequently developed at the sites of wound-producing injuries secondary to knife cut,[26] cement,[17] or splinter.[16]
Idiopathic SCC of the ventral fingers. SCC of the ventral finger has rarely been described in patients without an apparent tumor-associated risk factor. One patient had a verrucous carcinoma[29] and another patient had a pigmented SCC in situ that clinically mimicked malignant melanoma.[5]
Verrucous carcinoma of the ventral fingers. Verrucous carcinoma of the skin (also referred to as epithelioma cuniculatum or carcinoma cuniculatum) is a well-differentiated variant of SCC that is often clinically mistaken for a wart. Approximately 90 percent of these cutaneous tumors are located on the feet. However, albeit rare, they also have been observed to occur on the hands.[29] Verrucous carcinoma of the right palm and fourth finger developed in a 31-year-old construction worker,[29] and bilateral verrucous carcinoma of the ventral fingers was observed in an 81-year-old man with an associated syndactyly involving the third web space of both hands.14
Differential diagnosis of SCC of the ventral finger. Mimickers of SCC of the ventral finger are listed in Table 2.[5,13,16–18,20,23–25,29] In some of these individuals, the cancer was concurrently present or mimicked either a benign tumor, a malignant neoplasm, or a localized condition.
Verrucae or only viral changes have also been observed pathologically in the ventral digit SCC. Our patient had an intermittently painful tumor of five years duration that had progressively enlarged. A chronic wart was initially considered in the differential diagnosis; however, the tumor symptoms, size, and location prompted the clinician to perform a biopsy to exclude cancer. Although the initial specimen did not show wart or viral changes associated with the SCC, the excised residual tumor did reveal viral changes.
Treatment. The approach to therapy for SCC of the ventral digits is derived from the limited number of reported patients (Table 3).[5–14,16–18,20,21,23–26,29] Unsuccessful modalities were often described in individuals with advanced tumors. Many of the successfully treated patients—albeit some whose cancer diagnosis was significantly delayed—had amputation of the entire affected digit or en bloc removal of the digit at the joint proximal to the gross tumor involvement. Some of the patients with more extensive preoperative tumors also received postoperative tazarotene,[12] chemotherapy,[12] or radiation therapy[25] to prevent recurrence.
Local excision of the tumor, without the underlying tendons and bone, also provided eradication of the cancer. Our patient’s malignancy required five stages of Mohs surgery to completely remove the tumor based on microscopic evaluation of the tissue margins. His cancer demonstrates that unsuspected subclinical tumor extension and adjacent tumor invasion may be present in patients who have SCC of their ventral digits.
Alternative treatments for patients with less extensive SCC in situ of their palmar digits included photodynamic therapy[6,10,21] and ablation using the carbon dioxide laser.[7]
Response to therapy. Most of the patients with SCC in situ or SCC of a ventral digit—regardless of size or initial delay in diagnosis—have a favorable outcome.[5–10,12–14,17,18,20,21,23–25,29] Simple or more extensive resection of the tumor is usually curative. Subsequent local recurrence16 or metastases[16,26] of the tumor are uncommon.
Conclusion
SCC of the ventral digits is rare. Risk factors that may be associated with tumor development at this location in these individuals include local or systemic carcinogen exposure, congenital conditions, suppressed host immunity, coincident bacterial or viral infection, local radiation exposure, and trauma to the affected digit. Chronic dermatitis, epidermoid cyst, infection, keratoderma, melanoma, and/or verrucae are tumors and conditions that not only mimic but also can coincidentally occur at the site of palmar digit SCC. The mainstay of therapy is surgical removal of the cancer. This has been successfully performed by amputation of all or part of the affected digit or excision of the cutaneous malignancy with subsequent evaluation of margins to ensure complete removal of the tumor. The prognosis for patients with SCC of the ventral digits—regardless of the occasional delay in diagnosis, large tumor size, or both—is usually favorable following treatment of the cancer.
References
- Nordin P, Stenquist B, Hansson BG. Joint occurrence of human papillomavirus type 16 DNA in Bowen’s disease on a finger and in dysplasia of the vulva and the uterine cervix. [letter] Br J Dermatol. 1994;131:740.
- Alam M, Caldwell JB, Eliezri YD. Human papillomavirus-associated digital squamous cell carcinoma: literature review and report of 21 new cases. J Am Acad Dermatol. 2003;48:385–393.
- Gormley RH, Groft CM, Miller CJ, Kovarik CL. Digital squamous cell carcinoma and association with diverse high-risk human papillomavirus types. J Am Acad Dermatol. 2011;64:981–985.
- Lecerf P, Richert B, Theunis A, Andre J. A retrospective study of squamous cell carcinoma of the nail unit diagnosed in a Belgian general hospital over a 15-year period. J Am Acad Dermatol. 2013;69:253–261.
- Firooz A, Farsi N, Rashighi-Firoozabadi M, Gorouhi F. Pigmented Bowen’s disease of the finger mimicking malignant melanoma. Arch Iranian Med. 2007;10:255–257.
- Wong WT, Sheu H-M, Lee JY-Y, Fletcher RJ. Photodynamic therapy for Bowen’s disease (squamous cell carcinoma in situ) of the digit. Dermatol Surg. 2001;27:452–456.
- Tantikun N. Treatment of Bowen’s disease of the digit with carbon dioxide laser. J Am Acad Dermatol. 2000;43:1080–1083.
- Bonfiglio M, Landas S. Case report 640: well-differentiated, primary squamous cell carcinoma of the thumb. Skeletal Radiol. 1990;19:599–601.
- Chaimers RL, Ikram S, Schreuder F. Multiple digital squamous cell carcinoma due to ‘soluble-oil’. [clinical tip] J Plast Reconstr Aesthet Surg. 2008;10:1147.
- Souza CS, Felicio LBA, Bentley MV, et al. Topical photodynamic therapy for Bowen’s disease of the digit in epidermolysis bullosa. [letter]. Br J Dermatol. 2005;153:672–674.
- Hosokawa K, Yoshitatsu S, Kakibuchi M, et al. Simultaneous manifestations of squamous cell carcinoma in identical twins with epidermolysis bullosa. Plast Reconstr Surg. 1998;102:448–449.
- Sekar SC, Srinivas CR. Huriez syndrome. Indian J Dermatol Venereol Leprol. 2008;74:409–410.
- Watanabe E, Takai T, Ichihashi M, Uede M. A nonfamilial Japanese case of Huriez syndrome: p53 expression in squamous cell carcinoma. Dermatology. 2003;207:82–84.
- Lam WL, Hardwicke J, Laitung G. Squamous cell carcinoma in bilateral untreated syndactyly. Scan J Plast Surg Hand Surg. 2009;43:294–295.
- Ibe MM, Kawase M, Ishiji T, Kamide R, Niimura M. A cardiac allograft recipient with Bowen’s disease on a finger and concurrent perianal bowenoid papulosis. J Dermatol. 2003;30:389–394.
- Rauh MA, Duquin TR, McGrath BR, Mindell ER. Spread of squamous cell carcinoma from the thumb to the small finger via the flexor tendon sheaths. J Hand Surg. 2009;34A:1709–1713.
- Fisher J, Masson J, Rosen R. Squamous cell carcinoma of the hand masquerading as a cutaneous infection. Australasian J Dermatol. 2006;47:55–56.
- St-Amand H, Gaudreau G, Brutus J-P. Re: human papilloma virus-induced Bowen’s disease of the finger. [letter] J Hand Surg Eur Vol. 2008;33:385.
- Kettler AH, Rutledge M, Tschen JA, Buffone G. Detection of human papillomavirus in nongenital Bowen’s disease by in situ DNA hybridization. Arch Dermatol. 1990;126:777–781.
- Capretti AM, Terrana T. Clinical case: spinocellular carcinoma of the hand. Oncological considerations and reconstructive surgery. La Chirurgia degli organi di movimento. 2004;89:87–94.
- Guillen C, Sanmartin O, Escudero A, et al. Photodynamic therapy for in situ squamous cell carcinoma on chronic radiation dermatitis after photosensitization with 5-aminolaevulinic acid. J Eur Acad Dermatol Venereol. 2000;14:298–300.
- Kopelson PL, Nguyen QH, Moy RL. Veruca vulgaris and radiation exposure are associated with squamous cell carcinoma of the finger. J Dermatol Surg Oncol. 1994;20:38–41.
- Nelson MC, Stull MA, Lack EE, Bogumill GP. Case report 600: Post-radiation dermatitis with radiation-induced squamous cell carcinoma (well differentiated) of right third finger. Skeletal Radiol. 1990;19:150–153.
- Uchida K, Miyazaki T, Nakajima H, et al. Cutaneous squamous cell carcinoma (SCC) arising in stump of amputated finger in a patient with resected glossal SCC. BMC Research Notes. 2012;5:595.
- Davies MS, Nicholson AG, Southern S, Moss AHL. Squamous cell carcinoma arising in a traumatically induced epidermal cyst. Injury: Int J of the Care of the Injured. 1994;25:116–117.
- Lifeso RM, Bull CA. Squamous cell carcinoma of the extremities. Cancer. 1985;55:2862–2867.
- Forslund O, Nordin P, Hansson BG. Mucosal human papillomavirus types in squamous cell carcinomas of the uterine cervix and subsequently on fingers. Br J Dermatol. 2000;142:1148–1151.
- Forslund O, Nordin P, Andersson K, et al. DNA analysis indicates patient-specific human papillomavirus type 16 strains in Bowen’s disease on fingers and in archival samples from genital dysplasia. Br J Dermatol. 1997;136:678–682.
- Gertler R, Werber K-D. Management of verrucous carcinoma of the hand: a case report. Int J Dermatol. 2009;48:1233–1235.

