The editors of JCAD are pleased to present this biannual column as a means to recognize select medical students, PhD candidates, and other young investigators in the field of dermatology for their efforts in scientific writing. We hope that the publication of their work encourages these and other emerging authors to continue their efforts in seeking new and better methods of diagnosis and treatments for patients in dermatology.
J Clin Aesthet Dermatol. 2019;12(6):60–62
 by Vicky Yu, BS; Margit Lai Wun Juhász, MD; and Natasha Atanaskova Mesinkovska, MD, PhD
by Vicky Yu, BS; Margit Lai Wun Juhász, MD; and Natasha Atanaskova Mesinkovska, MD, PhD
Ms. Yu is with the University of Cincinnati College of Medicine in Cincinnati, Ohio. Drs. Juhász and Mesinkovska are with the Department of Dermatology at the University of California Irvine in Irvine, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
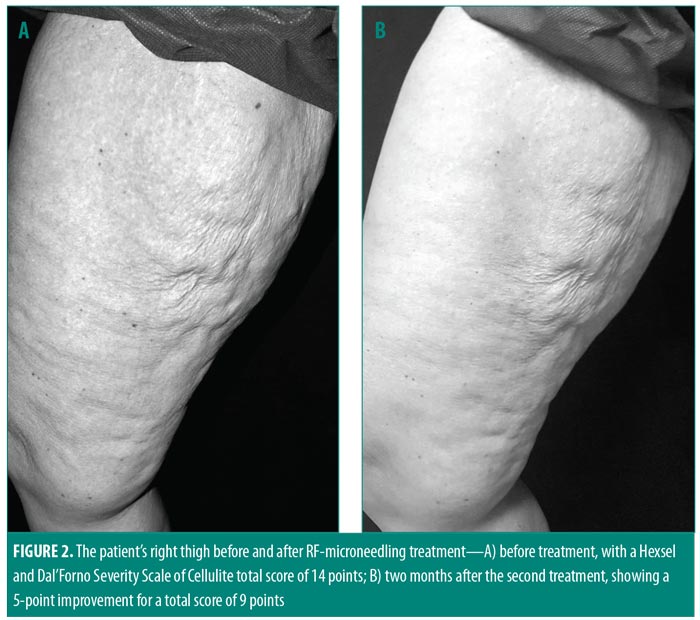
ABSTRACT: Radiofrequency (RF) microneedling has been used to reduce skin laxity, due to aging, on the face and neck. Our objective for this case study was to evaluate the use of RF in combination with microneedling to nonsurgically improve skin laxity, a result of significant weight loss, on the thighs of a 39-year-old woman. Two sessions of subcutaneous RF microneedling were performed five months apart on the patient’s bilateral medial thighs. Laxity was graded before the first session and two months following the second session using the Hexsel and Dal’Forno Severity Scale of Cellulite. Upon visual evaluation, the appearance of cellulite and skin laxity was improved, with a five-point improvement on the Hexsel and Dal’Forno scale at two months after the second treatment. Laxity and depth of depressions showed the most improvement. Our patient reported satisfaction with the results. RF microneedling might offer an effective alternative to surgical correction of skin laxity. Further research is needed to explore the expanding applications of RF microneedling in aesthetic medicine.
KEYWORDS: Radiofrequency, microneedling, laxity, body contouring, surgery, weight loss
With the increasing demand for noninvasive skin rejuvenation and body contouring procedures, novel radiofrequency (RF) systems and similar technologies have become some of the fastest-growing areas of aesthetic medicine. RF is a minimally invasive, nonablative technique that is commonly used for body contouring, skin tightening, and cellulite reduction.1 The electromagnetic technology is based on the use of an oscillating electrical current that generates and delivers thermal energy to the deep dermis and subcutaneous fat that stimulates the production of collagen, elastin, and hyaluronic acid, resulting in skin tightening and lifting, while causing minimal damage to superficial structures of the skin.1,2
Several modalities, both invasive and noninvasive, exist for the treatment of skin laxity of the arms and legs. Cosmetic surgery is the classical approach to reducing thigh skin laxity; however, there is a risk for linear surgical scarring using this method that some patients might find aesthetically unpleasing.3 Ultrasound, RF, and cryolipolysis have emerged as nonsurgical alternatives for the treatment of skin laxity; however, though these modalities require less down time by the patient compared to surgery, typical results using these methods have not yet achieved the same level of efficacy as surgical techniques.2
RF can be delivered at a frequency ranging from 3GHz to 24GHz using monopolar, bipolar, or unipolar devices, which allows for varying levels of depth penetration.1 To achieve greater efficacy, a new device that combines fractional RF (a subset of bipolar delivery) with microneedling has been developed as a nonsurgical means to reduce skin laxity, primarily on the face and neck.4 We present a case in which this new RF microneedling device was successfully used to treat thigh skin laxity, secondary to weight loss, and dimpling in an adult female patient.
Case Presentation
A 39-year-old woman with Fitzpatrick Skin Type II presented to the dermatological clinic with skin laxity and cellulite of the thighs attributed to significant weight loss. The patient had lost 47.7kg (105lbs) over the previous four years with diet and exercise. The patient previously had been treated by our clinic for alopecia totalis, which was stabilized with 5mg of tofacitinib twice daily. The current visit by patient was prompted following consultation with the surgery department regarding treatment of her thigh skin laxity and cellulite. Wishing to avoid the risks associated with an invasive cosmetic procedure, including the risk of scarring, the patient requested our consultation regarding alternative nonsurgical treatment modalities for skin laxity and cellulite.
The patient was assessed using the Hexsel and Dal’Forno Severity Scale of Cellulite and the Nürnberger-Müller Classification Scale.5,6 Although the Nürnberger-Müller classification is considered the current standard in classification of cellulite, it is less detailed than the newer Hexsel and Dal’Forno Severity Scale of Cellulite. The Hexsel and Dal’Forno Severity Scale of Cellulite uses a 0-to-3 numerical score (0=none, 1=mild, 2=moderate, 3=severe) to rate five categories: number of evident depressions (0 to 10 or more); depth of depressions (0=no depressions, 3=deep depressions); morphological appearance of skin surface alterations (0=no raised areas, 3=“orange peel,” “cottage cheese,” or “mattress” appearance); and grade of laxity/flaccidity (0=slight, 3= severe draped appearance). The Hexsel and Dal’Forno Severity Scale of Cellulite also includes the Nürnberger-Müller Classification Scale grade (Grades 0–III). The Nürnberger-Müller Classification Scale designates grades as the following: Grade 0=no alteration of skin surface; Grade I=alterations to skin surface only seen by pinching or contracting the skin; Grade II=”orange peel” or “mattress” appearance evident when standing with no skin manipulation; and Grade III=findings of Grade II plus the presence of raised areas or nodules.
Our patient’s initial score comprised the following: number of evident depressions=3 points; depth of depressions=3 points; morphological appearance of skin surface alterations=3 points; laxity=2 points; and Grade III for the Nürnberger-Müller classification=3 points, for a total score of 14.7 Following the assessment, cryolipolysis was ruled out as a treatment method due to the patient’s level of skin laxity. RF microneedling was ultimately selected as the most appropriate nonsurgical treatment for our patient’s thigh skin laxity and cellulite.
Two sessions of subcutaneous RF microneedling (PROFOUND™, formally known as ePrime™ or Evolastin™; Syneron Medical Ltd., Irvine, California) were performed five months apart on the bilateral medial thighs of the patient. An area of skin laxity measuring 15cm×15cm on each thigh was cleansed and anesthetized with 0.5% lidocaine with epinephrine. RF microneedling was administered in two passes, one vertical and one horizontal, for a total of 235 RF injections at a depth of 5.8mm, with the device set at 67°C, four seconds, and pulses administered 5mm apart at a frequency of 5±460 kHz (Figure 1). The parameters were kept the same for the second session five months later, with 214 RF injections.

Reported side effects included superficial ecchymosis and erythema, which resolved 3 to 5 days postprocedure without further medical intervention.
The patient was visually assessed twice—five months after the first treatment and two months after the second treatment—by two blinded dermatologists using pre- and post-procedure images. Based on the Hexsel and Dal’Forno Severity Scale score, the appearances of cellulite and skin laxity were rated as improved following the first treatment. Following the second treatment, the score for number of evident depressions remained unchanged (3 points), but the scores for depth of depressions and skin laxity improved by one point and morphological appearance of skin surface alterations and Nürnberger-Müller classification improved by two points, resulting in a total five-point reduction in the Hexsel and Dal’Forno Cellulite Scale score and a new total score of nine points (Figure 2). The patient reported satisfaction with the results.
Discussion
Although RF’s exact mechanism of action for improving skin laxity and appearance of cellulite has not been clearly defined, the main hypothesis centers around RF’s ability to induce denaturation, contraction of collagen fibers, and neocollagenesis, causing tissue retraction that clinically translates to “tightening” of skin and superficial tissues.4 Several studies have reported the efficacy of RF (even without microneedling) for these purposes.8
Manuskiatti et al8 reported a mean 50-percent improvement in cellulite appearance in 37 patients with Grade 2 or higher cellulite of the thighs, arms, buttocks, and abdomen following eight RF treatments without microneedling (1 MHz, 40–42°C). A significant decrease in abdomen and thigh circumference was also reported, as was a mean reduction of 10.5 percent in the thickness of adipose tissue, measured by ultrasound, suggesting RF’s efficacy in fat reduction.
RF combined with microneedling for skin tightening has primarily been used for face and neck skin laxity secondary to aging. In a study evaluating the effectiveness of RF microneedling on skin laxity in 42 patients (mean age 55 years), Alexiades-Armenakas et al9 reported a 95-percent response rate,with a mean improvement of 24.1 percent, at six months. For this study, the authors used their own rating scale, the Alexiades-Armenakas Rhytid and Laxity Grading Scale, which utilizes 0-to-4 scoring method in half-point increments.10 Additionally, a randomized, controlled study by Alexiades-Armenakas et al2 evaluating the effectiveness of RF microneedling on skin laxity of the face and neck reported a 16-percent improvement in 15 female patients (mean age 60 years) compared to a 49-percent improvement in patients who underwent surgical facelifts.2
Conclusion
Although RF microneedling has not yet achieved the same level of efficacy as surgery in the treatment of skin laxity and cellulite, RF appears to provides a safe, noninvasive treatment option for those patients who wish to avoid surgery. Generally, patients undergoing treatment with RF microneedling can expect minimal pain and downtime, no scarring, and only mild, transient bruising, erythema, and edema.8
References
- Weiss RA. Noninvasive radio frequency for skin tightening and body contouring. Semin Cutan Med Surg. 2013;32(1):9–17.
- Alexiades-Armenakas M, Rosenberg D, Renton B, et al. Blinded, randomized, quantitative grading comparison of minimally invasive, fractional radiofrequency and surgical face-lift to treat skin laxity. Arch Dermatol. 2010;146(4):396–405.
- Hurwitz DJ. Thighplasty in the weight loss patient. Semin Plast Surg. 2006;20(1):38–48.
- Lolis MS, Goldberg DJ. Radiofrequency in cosmetic dermatology: a review. Dermatol Surg. 2012 Nov;38(11):1765-1776.
- Hexsel DM, Dal’forno T, Hexsel CL. A validated photonumeric cellulite severity scale. J Eur Acad Dermatol Venereol. 2009;23(5):523–528.
- Nürnberger F, Müller G. So-called cellulite: an invented disease. J Dermatol Surg Oncol. 1978;4(3):221–229.
- Hexsel DM, Dal’forno T, Hexsel CL. A validated photonumeric cellulite severity scale. J Eur Acad Dermatol Venereol. 2009;23(5):523–528.
- Manuskiatti W, Wachirakaphan C, Lektrakul N, Varothai S. Circumference reduction and cellulite treatment with a TriPollar radiofrequency device: a pilot study. J Eur Acad Dermatol Venereol. 2009;23(7):820–827.
- Alexiades-Armenakas M, Newman J, Willey A, et al. Prospective multicenter clinical trial of a minimally invasive temperature-controlled bipolar fractional radiofrequency system for rhytid and laxity treatment. Dermatol Surg. 2013;39(2): 263–273.
- Alexiades-Armenakas M. Rhytides, laxity, and photoaging treated with a combination of radiofrequency, diode laser, and pulsed light and assessed with a comprehensive grading scale. J Drugs Dermatol. 2006 Sep;5(8):731–738.

