J Clin Aesthet Dermatol. 2019;12(3):40–43
 by Bruna Paninson, MD; Beatriz Moritz Trope, MD, PhD; Julio César Moschini, MD; Maria Auxiliadora Jeunon Sousa, MD; and Marcia Ramos-e-Silva, MD, PhD
by Bruna Paninson, MD; Beatriz Moritz Trope, MD, PhD; Julio César Moschini, MD; Maria Auxiliadora Jeunon Sousa, MD; and Marcia Ramos-e-Silva, MD, PhD
Drs. Paninson, Trope, and Ramos-e-Silva are with the Sector of Dermatology, Postgraduation Course in Dermatology at the University Hospital and School of Medicine, Federal University of Rio de Janeiro in Rio de Janeiro, Brazil. Dr. Moschini is in private practice in Rio de Janeiro, Brazil. Dr. Sousa is with Investigações Diagnósticas Inc. in Rio de Janeiro, Brazil.
FUNDING: No funding was received for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: The nevus sebaceous of Jadassohn, usually present at birth, is a hamartoma composed predominantly of sebaceous glands, which can progress to benign and malignant tumors. Malignant neoplasms on the nevus sebaceous occur in about 2.5 percent of cases, with basal cell carcinoma accounting for 1.1 percent. Suspected cases of transformation should be clinically monitored and excised. We report the case of a 38-year-old man with a yellowish plaque located in the left parietal region, present from birth, on which a brownish papular lesion developed. The histopathological examination showed that it was a basal cell carcinoma. In presenting this case of basal cell carcinoma on a nevus sebaceous, we emphasize the evolutionary possibilities in order to improve prompt diagnosis and correct treatment.
KEYWORDS: Nevus sebaceous of Jadassohn, nevus sebaceous, basal cell carcinoma
Introduction
Nevus sebaceous, also called nevus sebaceous of Jadassohn or organoid nevus, is a benign skin malformation.1 Considered to be rare, it is responsible for up to 0.2 percent of dermatological appointments.2 The lesions can be present at birth or appear in early childhood, with similar prevalence in both sexes, and occasionally with a positive familial history.
A nevus sebaceous initially presents as a flat plaque of yellowish coloration that later thickens and becomes mamillonated and verrucous. It can evolve into malignant lesions, especially in adults, leading some authors to suggest surgical treatment during adolescence.1
Histologically, a nevus sebaceous is characterized by papillomatous hyperplasia of the epidermis and sebaceous glands.3 Some neoplasias can entail a transformation of the nevus lesion, with basal cell carcinoma (BCC) among them. Recent etiopathogenic studies point to an association with human papilloma virus (HPV) or patched gene mutations.4
Case Presentation
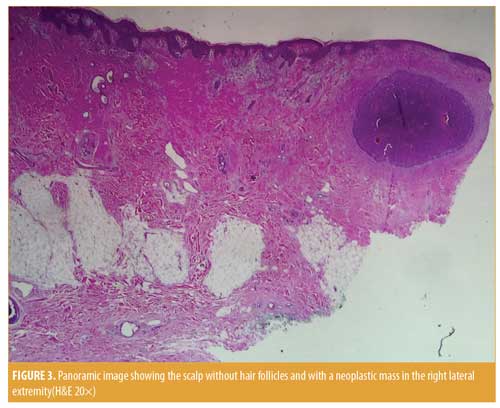
During a routine medical appointment, a brownish papule was observed on the scalp of a 38-year-old Caucasian man, a native of Rio de Janeiro, Brazil. He reported that it had been present for many years. Previous histopathology, provided to us by the patient, revealed a BCC. The patient requested a consultation with our team. During the dermatological examination, an elliptical, pinkish-yellowish plaque with a flat mamillonated surface was observed on the left parietal region of the scalp. Local alopecia was present. On one of the lateral borders, a more papulous lesion near the surgical scar from the previous biopsy was observed (Figure 1). The patient stated that this yellowish lesion, which he regarded as a “mole,” had been present since birth.
With the diagnostic impression that BCC had developed on a nevus sebaceous, the lesion was completely excised by surgery, with subsequent simple closure by suture. The patient recovered fully and remained without complications after a follow-up period of 18 months.

Discussion
Nevus sebaceous of Jadassohn is a congenital hamartoma of the epidermis, dermis, and appendages with a prevalence of sebaceous elements frequently occurring on the scalp. Nevus sebaceous is often associated with focal alopecia, similar to our presented case. Other common sites include the face and neck.
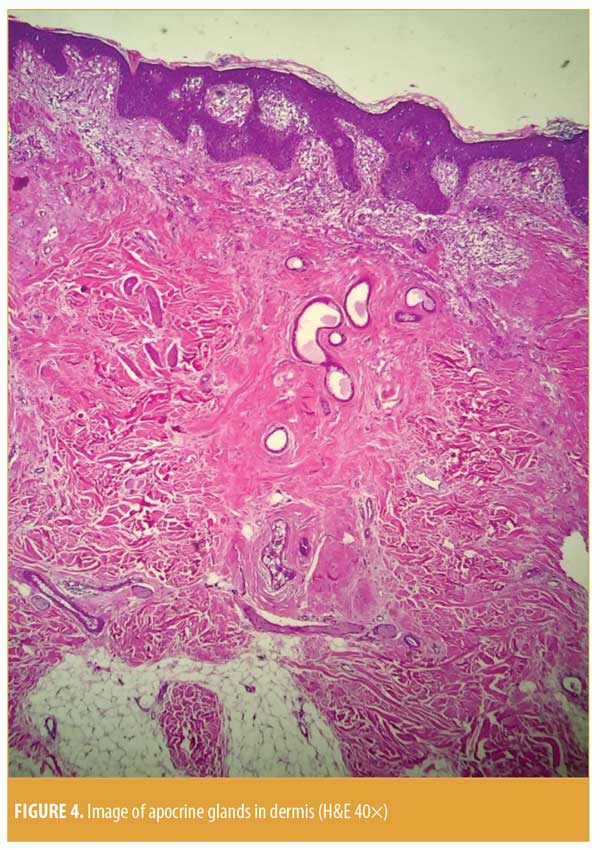
A nevus sebaceous can reach a diameter of 10cm and develops in three stages.5 The first stage, ranging from birth to childhood, is characterized by a flat lesion with a soft surface at touch and yellowish-pink coloration, remaining unchanged due to quiescence of the sebaceous glands. With the onset of adolescence comes the second stage, when the lesion becomes vegetating and mamillonated with an increase in thickness due to hormonal influence on the sebaceous and apocrine glands. The third stage, occurring in about 20 percent of cases, usually develops after the age of 40 years, and emergence of tumors such as trichoblastoma, syringocystadenoma papilliferum, and trichilemmoma might occur.2,6
Malignant neoplasia occur in 2.5 percent of the cases and are considered rare, with BCC (1.1%), squamous cell carcinoma (0.57%), sebaceous carcinoma, and apocrine carcinoma among them.2 BCC is the most common of the superposing malignant tumors. However, more recent research suggests that many of the cases previously thought to be BCC might actually be trichoblastoma; thus, the incidence of BCC might be closer to 0.8 percent.7
Etiology of BCC on an organoid nevus is unknown, but recent studies point to a link to HPV. The oncogenicity of HPV is yet to be determined. Research has shown that the virus interacts with certain cell proteins, altering their expression levels and functions. Some proteins are also overexpressed in BCC. The high expression of p16INK4a and pAkt2 is frequently associated with the presence of some beta HPVs such as HPV15. The involvement of HPV in the carcinogenesis of some BCC subtypes is suggested by the activation of those proteins and the presence of that virus. However, the reflex of this involvement on the biologic behavior of those BCCs has yet to be determined.8,9
Other risk factors related to BCC oncogenesis include a lighter skin phototype (Fitzpatrick Skin Types I and II); positive familial BCC history (30–60%); freckles in childhood; frequent exposure to ultraviolet (UVA) radiation without appropriate sun protection; frequent sunburns during youth; radiotherapy; phototherapy (photochemotherapy and UVB); arsenic exposure; use of dark hair dyes; a high-fat diet high; use of tanning beds; prolonged use of photosensitizing medications (e.g., tetracyclines, sulfonamides, fluoroquinolones, phenothiazines, or diuretics); exposure to paraffin, coal, coaltar, tar, industrial oils, agricultural defensives, pesticides, or ionizing radiation; and presence of chronic scars (e.g., occurring from burns, discoid lupus, vaccines, or tattoos). The influence of smoking and alcohol addiction remain controversial.10
The presence of nevus sebaceous of Jadassohn is a risk factor, regardless of the presence of BCC, and many researchers consider it a premalignant lesion.5 A rapid or circumscribed increase in size, as well as the onset of a pigmented lesion or superposed ulceration, should raise suspicion of malignant transformation. The superficial and nodular types of BCC can produce pigments. Our patient’s history revealed that he had a brownish lesion overlying the nevus sebaceous surgically removed, which raised our suspician of BCC and was confirmed by histopathology (Figures 2–5). The malignant tumors that emerge from organoid nevi are usually of low aggression; however, some authors report highly aggressive tumors.1


Surgical excision is presently only recommended in the case of a suspected malignancy, but prophylactic excision in adolescence is also acceptable following an evaluation of the extension, location, and aesthetics of the lesion.11 Reconstruction with grafts and rotations is sometimes necessary due to tissue loss, but this was not necessary in our patient. Clinical follow-up is imperative for patients in whom the lesions are not removed. Alternative treatment options include photodynamic therapy, CO2 laser, and dermabrasion. Since these treatment modalities do not completely eliminate the lesion, the risk of recurrence and potential development of neoplasia remains.
Conclusion
We present a rare case of nevus sebaceous of Jadassohn that progressed to BCC in an adult man. Histopathologic results indicated the presence of tumor remaining on the borders of the previous surgical resection. We performed a complete excision of the lesion, closing with simple suture.
We emphasize the need for regular follow-up in patients with nevus sebaceous. Due to the risk of malignant neoplasia developing from nevus sebaceous, clinicians should be suspicious of any changes in this rare skin malformation. Histopathological examination should be used to confirm diagnosis. Surgical excision is recommended.
References
- Zanini M, Wulkan C, Paschoal LHC. [Organoid nevus or Jadassohn’s sebaceous nevus: a discussion]. Med Cutan Iber Lat Am. 2003;31(2):121–122. Article in Portuguese.
- Galvis KH, Frattini SCM, Fernandes KAP, et al. [Jadassohn’s sebaceous nevus]. RBM Dermatologia & Cosmiatria. 2015;71(2):23:25. Article in Portuguese.
- Rosen H, Schmidt B, Lam HP, et al. Management of nevus sebaceous and the risk of basal cell carcinoma: an 18-year review. Pediatr Dermatol. 2009;26(6):676–681.
- Rodrigues TNA, Galvão LEG, Gonçalves HS, Pontes MAA. [Basal cell carcinoma growth over a nevus sebaceous: treatment of the field cancerization with photodynamic therapy]. Surg Cosmetic Dermatol. 2017;9(1):100–103. Article in Portuguese.
- Moody MNL, Landau JM, Goldberg LH. Nevus sebaceous revisited. Pediatr Dermatol. 2012;29(1):15–23.
- Jardim MM, Souza BCE, Fraga RC, Fraga RC. Rare desmoplastic trichilemmoma associated with nevus sebaceous. An Bras Dermatol. 2017;92(6): 836–837.
- Kim JH, Park HY, Ahn SK. Nevus sebaceous accompanying secondary neoplasms and unique histopathologic findings. Ann Dermatol. 2011;23(Suppl 2):S231–S234.
- Pereira FB, Cuzzi T. [Basal cell carcinoma, chrysalides-like structures, oncogenes, and sebaceous nevus: some considerations]. Surg Cosmet Dermatol. 2012;4(1):97–99. Article in Portuguese.
- Paolini F, Carbone A, Benevolo M, et al. Human papillomaviruses, p16INK4a and Akt expression in basal cell carcinoma. J Exp Clin Cancer Res. 2011;30:108.
- Chinem VP, Miot HA. [Epidemiology of basal cell carcinoma]. An Bras Dermatol. 2011;86(2): 292–305. Article in Portuguese.
- Enei ML, Paschoal FM, Valdés G, Valdés R. Basal cell carcinoma appearing in a facial nevus sebaceous of Jadassohn: dermoscopic features. An Bras Dermatol. 2012;87(4):640–642.

